Sivakami Rethnam Haug, Päivi Siukosaari, Jussi Furuholm and Malin Brundin
An evaluation of case difficulty, operator abilities, when and how to refer
Dr.odont. (Universitetet i Bergen), specialist in endodontics (University of Pennsylvania), associate professor. Department of Clinical Dentistry, University of Bergen, Norway.
Odont. dr, universitetslektor, Övertandläkare Endodonti. Institutionen för Ododontologi, Medicinska Fakulteten, Umeå Universitet, Sweden.
DDS, Specialist in Endodontics, Dental advisor, Patient Insurance Center.
DDS, PhD, University lecturer. Department of Oral and Maxillofacial Diseases, University of Helsinki, University of Helsinki.
Headlines
Endodontically treated tooth needs to last a lifetime and therefore root canal treatment has to be performed with precision the first time around.
A good knowledge of case difficulty and operator abilities can help DP decide on whether they want to treat a tooth or refer to a specialist.
The Nordic Endodontic Assessment Form places DP and treatment tooth into 4 categories A, B, C and D according to technical skills, theoretical knowledge, and use of tools by DP.
To make a referral, good communication with the patient is essential.
The referral needs to be done early in the treatment procedure.
Dental practitioners (DP) often perform endodontic treatment on teeth that are difficult and challenging. Endodontic treatment is sometimes associated with treatment related problems such as mishaps, procedural errors, iatrogenic errors, complications, accidents and in serious cases, malpractice. These mishaps in general are closely linked to case difficulty. Endodontics is the leading cause of dental malpractice claims. A new case difficulty evaluation form, the Nordic Endodontic Assessment Form is introduced here. This form places DP and tooth into 4 categories according to technical skills, theoretical knowledge and use of tools. Category A DP does not use magnification tools. Category B DP use some form of magnification aid, have experience in performing endodontic therapy, and complementary theoretical knowledge. Category C DP use dental loupes, has experience and special interest in Endodontics. Category D DP are either an Endodontists or DP with special training in Endodontics who use the dental operating microscope. With this Nordic Endodontic Assessment Form, DP can self-evaluate which category the tooth that needs treatment belongs, identify case difficulty and refer patients when there is a need for it. How to write a referral and what should be included is also discussed.
People prefer to keep their natural teeth throughout their lifetime. This demand has led to dental practitioners (DP) performing endodontic treatment on teeth that is difficult and challenging to treat. Endodontic treatment improves quality of life. Unfortunately, endodontic treatment performance is sometimes associated with treatment related problems. These problems are referred to as mishaps, procedural errors, iatrogenic errors, complications, accidents and in serious cases, malpractice. Endodontic mishaps in general are closely linked to case difficulty which may or may not have an effect on treatment outcome depending on the diagnosis and type of mishap [1]. Endodontic mishaps, procedural errors or iatrogenic injury can also be interpreted to be a result of ignorance or deficiency of knowledge [1]. On the other hand, accidents are injury caused by operators, for example ‘sodium hypochlorite’ accident. Complications can be due to any of the problems or patient related complications, for example allergic reactions [2][3]. Malpractice is defined as illegal, improper, or negligent professional behavior. Unfortunately, endodontics is the leading cause of dental malpractice claims in certain countries [4].
When suspecting potential malpractice, the dental practitioner’s level of performance at each stage is reflected with the complexity of the case, and whether a general standard of care is achieved. The most harmful consequences are observed in injuries related to irrigants or medicaments in endodontics, such as sodium hypochlorite accident or extrusion of calcium hydroxide beyond the apical foramen to cause damage to the neural tissue or sinus causing complications (figure 1A and B) [5][6]. These accidents are often evaluated as avoidable whereby DP have failed to follow the standard level of practice. However, fear of procedural errors or other endodontic mishaps should not deter clinicians from performing endodontic therapy [7].
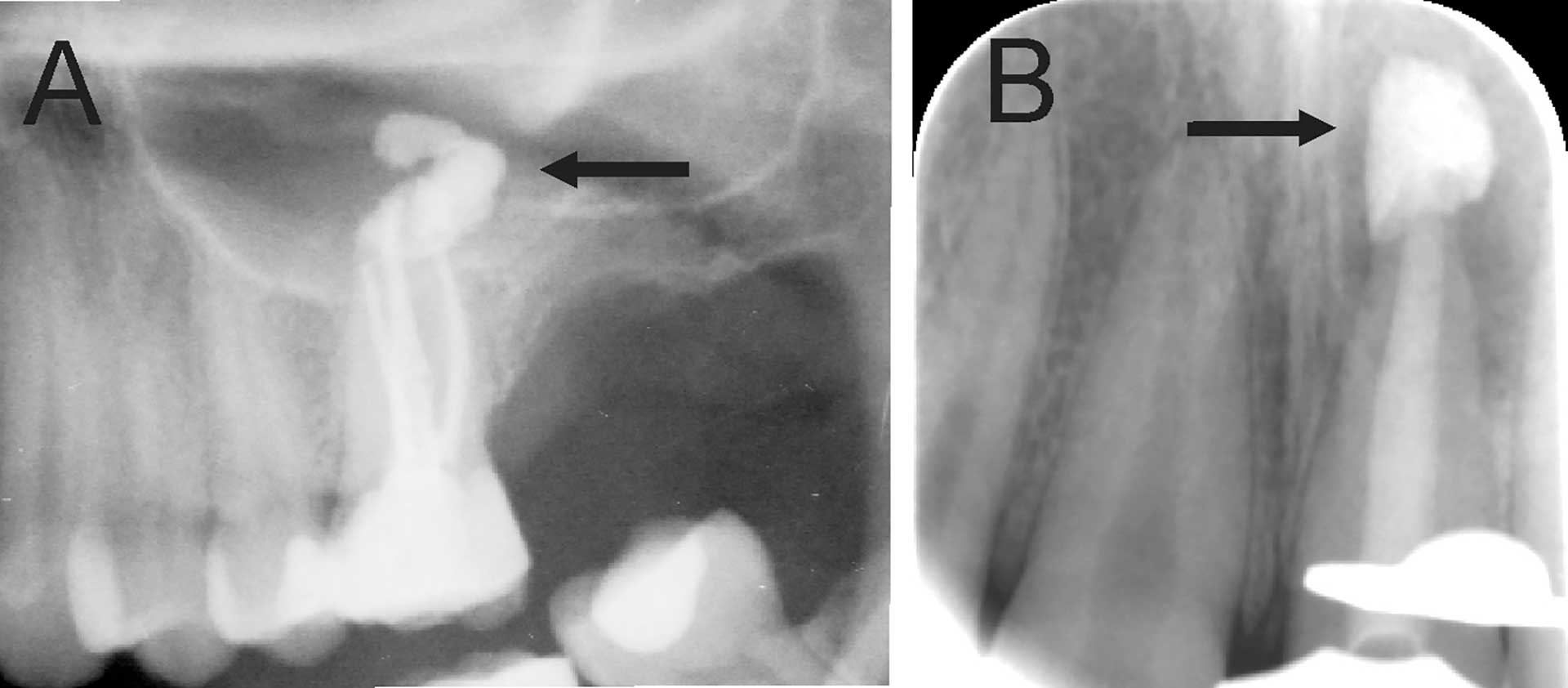
Figure 1. (A) An orthopantomography section showing Ca(OH)2 beyond the apical foramen of maxillary first into the maxillary sinus (arrow) and (B) a periapical radiograph with Ca(OH)2 extrusion beyond the apical foramen (arrow) of a central incisor which required surgical intervention.
Evaluation of case difficulty
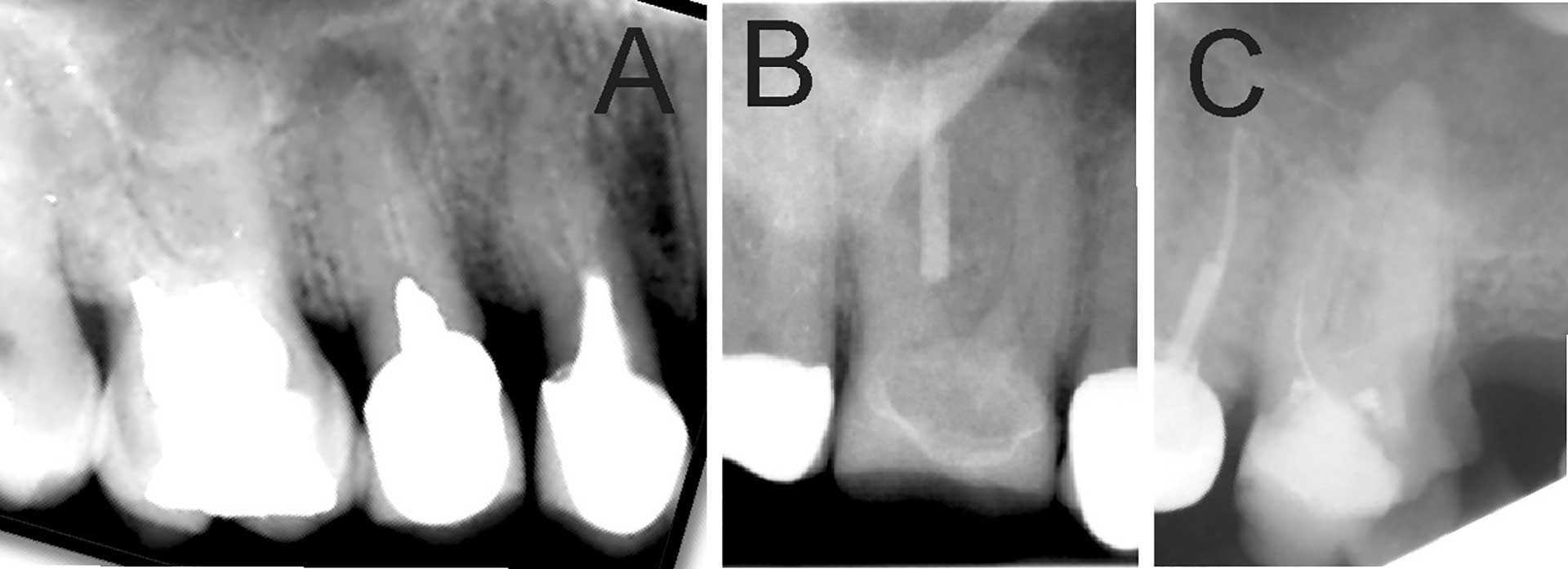
Figure 2. Previously treated tooth with no or inadequate root filling in canals. (A) Maxillary premolars with 3 roots inadequately filled and restored with post and crown. Maxillary first molar with no visible root filling with restoration in pulp chamber and coronal restoration (B) Maxillary first molar with visible root filling only in the palatal canal. (C) Inadequate root filling or missed root canal in maxillary first molar.
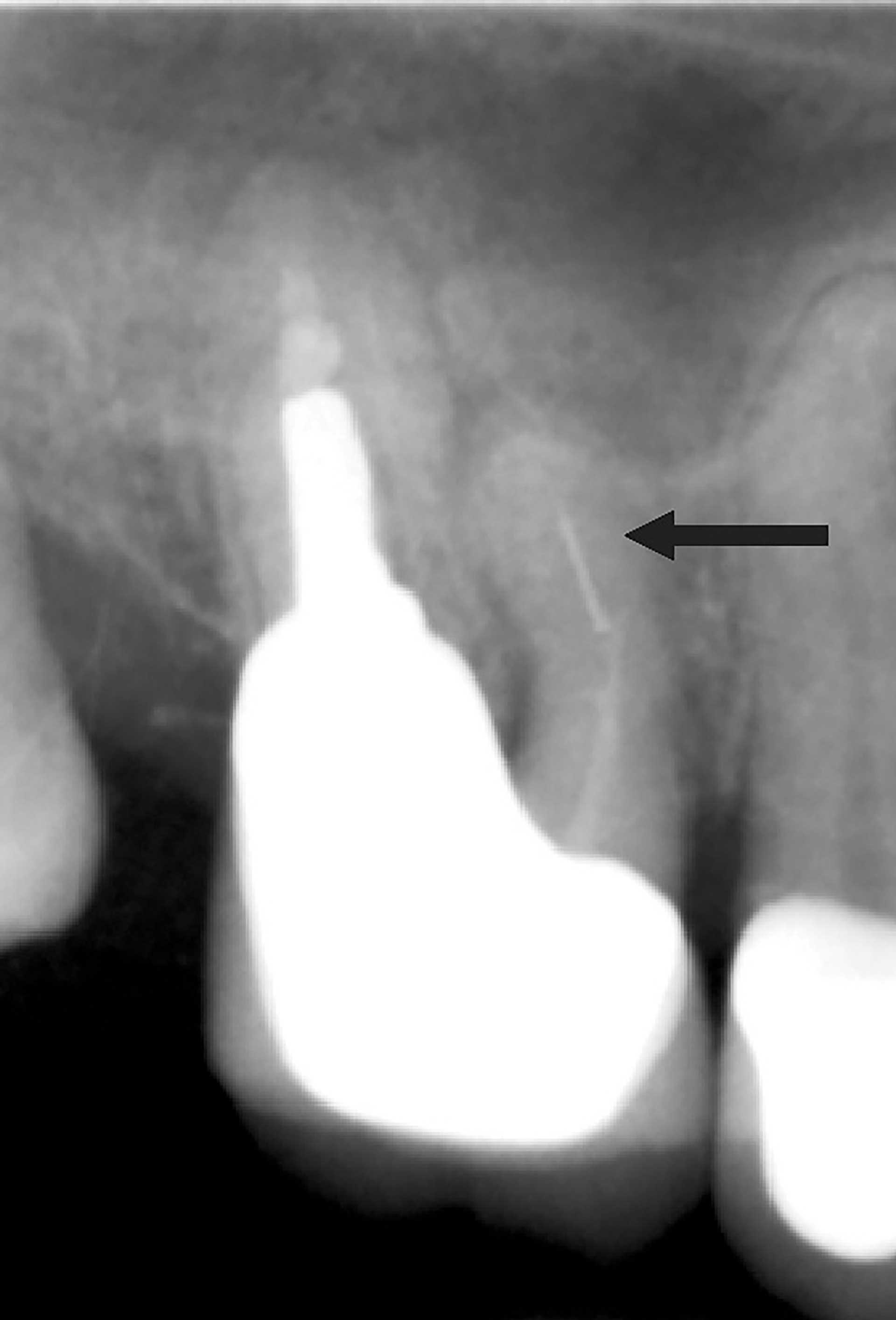
Figure 3. Radiograph of a previously root filled maxillary first molar with separated file in mesio-buccal canal (arrow).
Factors leading to endodontic problems can be preoperative or operative. Failure to understand root canal anatomy and misdiagnosis are preoperative factors leading to endodontic problems. There are numerous operative factors. One of these is failure to treat the root canal either because it was not localized, or the DP did not look for it ( figures2A-C)[8][9].The frequency of apical periodontitis is shown to be higher in teeth with at least one untreated missed root canal [10]. Accidental perforations frequently lead to tooth extraction and are generally avoidable with good endodontic practice [11]. Failure to completely instrument or obturate root canal either due to misjudged working length, creating obstructions such as instrument separation, ledge or zip formation can lead to persistence of infection. Endodontic files are susceptible to separation due to cyclic fatigue or torsional stress with a 1% overall incidence rate [12]. The most common location for instrument fracture is the apical part of a mesio-buccal root canal in a molar tooth (figure 3). Severe curvature of the canal increases the risk of file breakage [13]. Short obturation (<2 mm from radiographic apex) has reduced success rate similar to overfill with gutta percha [14].
The elderly patient
A systematic review of longitudinal root canal treatment (RCT) outcomes demonstrated that increased patient age does not reduce endodontic success. Age should not be considered by dentists or patients when making treatment decisions [15]. However, age-related changes in teeth may result in difficulty in performing RCT (figure 4A). A recent study showed that elderly needed RCT on teeth that had large restoration and full coverage crowns [16]. This adds to the difficulty level of tooth. Secondary dentine formation occurs throughout life reducing the dimension of pulp chamber and root canals resulting in difficulty during cavity preparation and canal localization for an operator [16] (figures 4B and C). Furthermore, calcified root canals in one study showed that all canals were accessible within a maximum of 60 min. The success rate after a follow-up of 3 years was 80% [17].
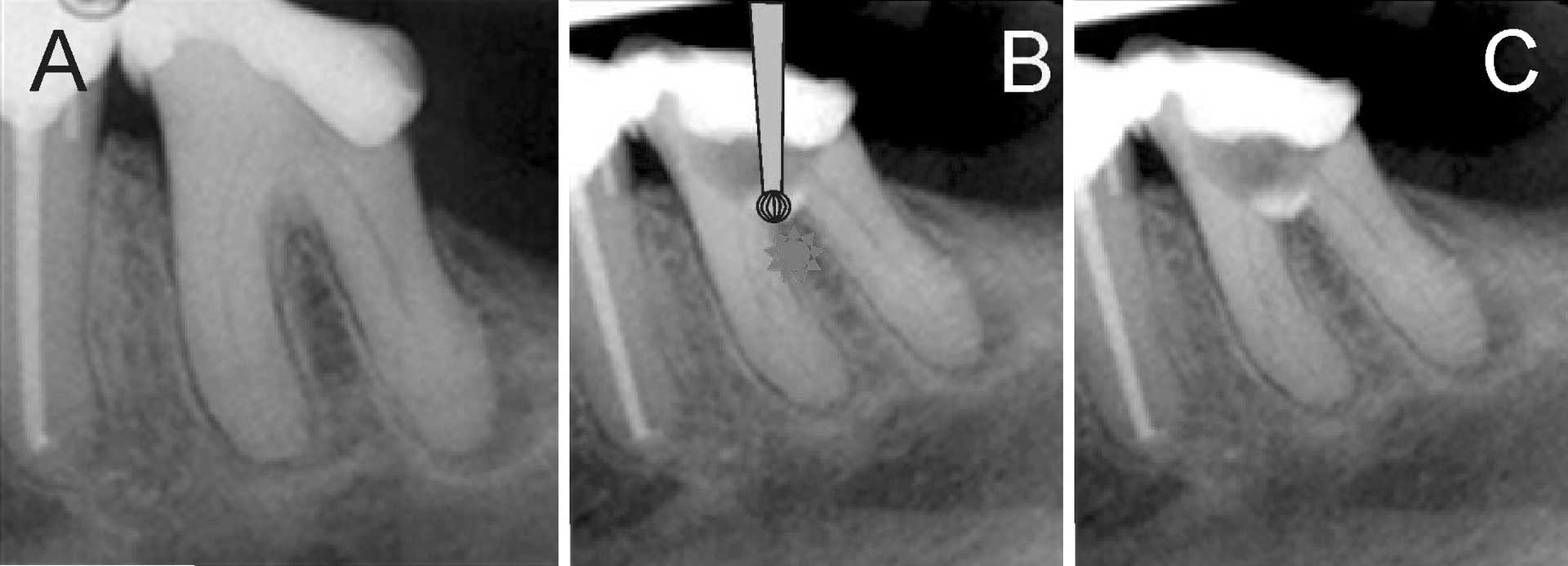
Figure 4. (A) Radiograph of mandibular left first molar in an elderly patient showing reduced pulp canal space. (B) Schematic illustration of bur in the furcation region with perforation in the furcation periodontium and overextended access preparation. An inadequate pre-operative assessment of radiograph led to this problem. (C) Restoration over furcation perforation.
Nordic Endodontic Assessment Form
There are many case difficulty evaluation forms [18]. The American Association of Endodontists case difficulty assessment form (AAE form) is commonly used both during dental education and by referring dentists [1][18][19]. Briefly, cases are categorized as easy, moderate and highly difficult. A recent study reported that teeth in high difficulty category, had significant more endodontic mishaps and number of treatment visits [1]. However, the AAE form has some shortcomings. For example, patients with certain medical conditions are placed in high difficulty category in the AAE form.
Operator Abilities
DP have a varied interests, knowledge, competence, and skills. Therefore, a new case difficulty assessment form, Nordic Endodontic Assessment Form based on the current AAE form is introduced here (Table 1). The Nordic Endodontic Assessment Form places DP and tooth needing treatment into 4 categories A, B, C and D according to technical skills, theoretical knowledge and use of tools by DP. It has been previously reported that although DP received similar undergraduate dental education, confidence and security when performing RCT was varied [20]. A short description of the 4 categories follows. The authors emphasis that this is a recommendation and not a rule.
Criteria |
A |
B |
C |
D |
|---|---|---|---|---|
Operator factors |
|
|
|
|
Treatment type and challenges |
|
|
|
|
Diagnosis |
|
|
|
|
Tooth type |
|
|
|
|
Tooth inclination |
None |
|
|
|
Tooth rotation |
None |
|
|
|
Crown morphology |
|
|
|
|
Radiographic appearance |
|
|
|
|
Root curvature |
|
|
|
Category A: DP do not use any magnification tools. Category A DP perform RCT sporadically but can upgrade to Category B with the use of magnification aids, keeping up-to-date with continuing dental education courses and reading current literature.
Category B: DP use some form of magnification aid, has experience in performing endodontic therapy, and has complementary theoretical knowledge. A newly graduated dentist who uses some form of magnification aid is in Category B.
Category C: DP use dental loupes and has experience and special interest in Endodontics. Undergraduate students currently treat patients in Category C under supervision [1].
Category D: DP use dental operating microscope and is able to interpret Cone Beam CT images to make appropriate treatment plan. Category D DP are either specialists in Endodontics or DP who have received special training and has interest in Endodontics.
The following is a short description with clinical cases describing why certain cases and conditions are placed in different categories. All DP should be able to perform emergency treatment on patients (category A). Category D DP can treat all treatment cases from A to D, category C DP can treatment A to C treatment cases, category B DP can treat A and B while a category A DP is advised to treat cases listed in category A. A DP can easily move up or down in these categories with experience, tools, through continuing educational courses and lifelong learning [21].
Diagnosis
Teeth with extensive differential diagnosis can be challenging for DP [19]. So, at least a category B DP should attempt to treat these teeth (figure 5 A-B).
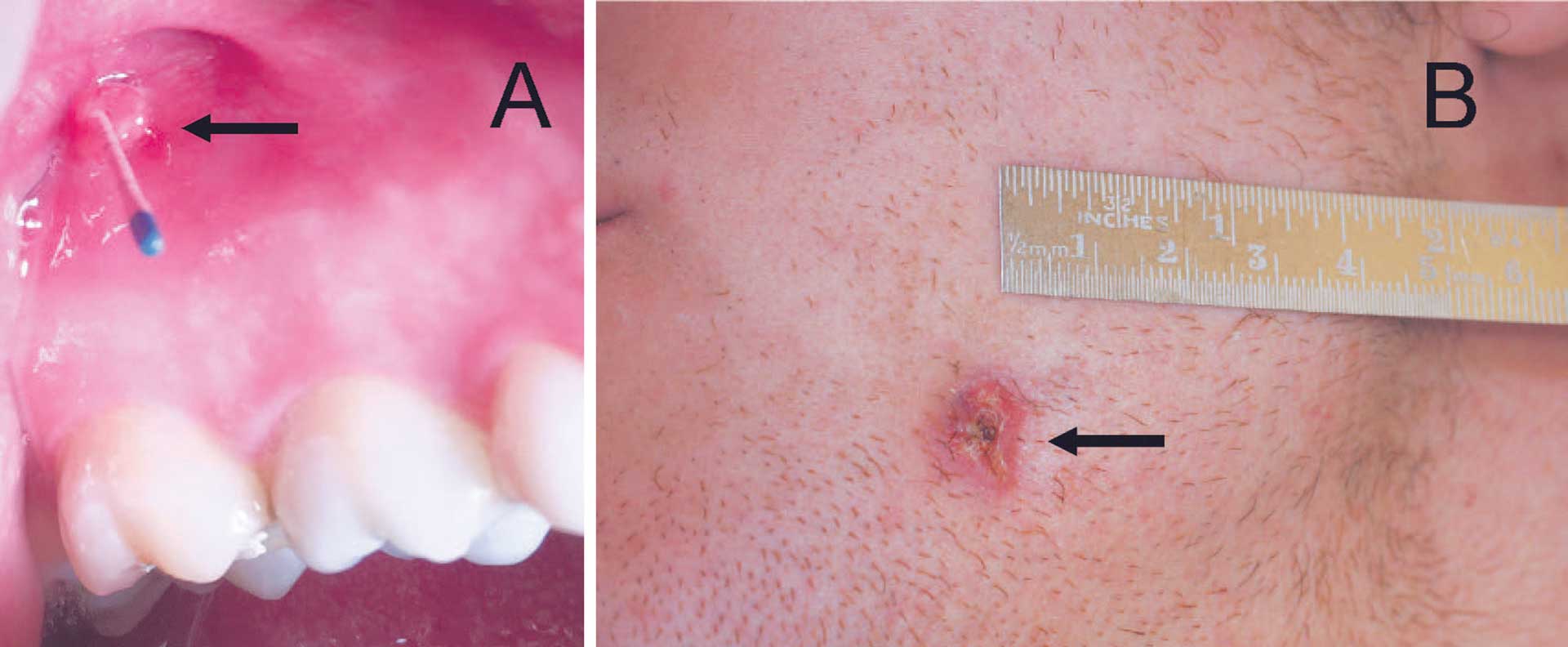
Figure 5. Fistula (arrows) can be located intraoral (A) and extraoral (B). Tracing the fistula with a gutta percha point leads to the source of infection. A radiograph with trace fistula is imperative for diagnosis.
A previously root filled tooth with apical periodontitis is complicated to treat because a new attempt needs additional theoretical knowledge, clinical skills and recall plan.
Tooth type
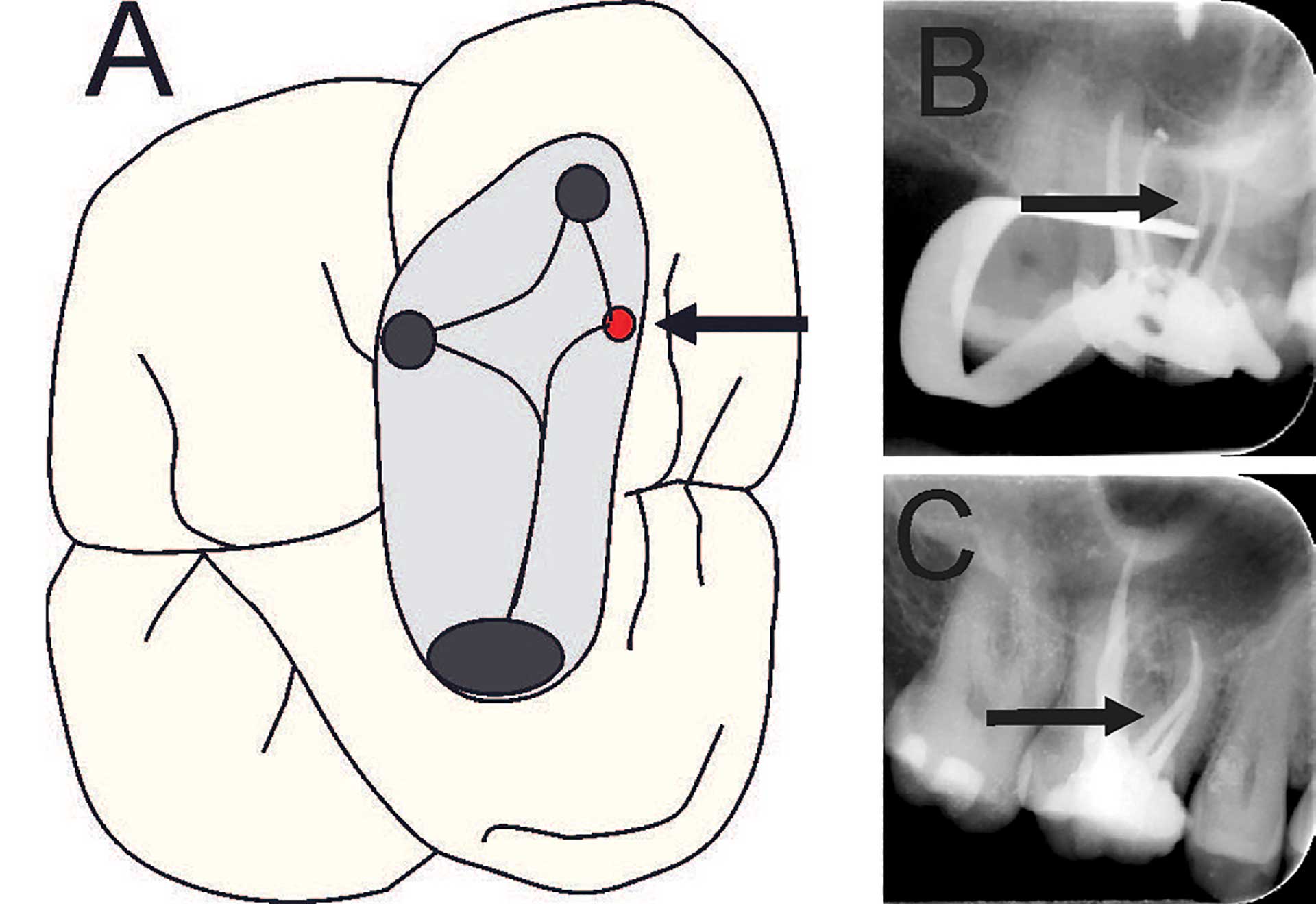
Figure 6. (A) Maxillary molar after access preparation. Arrow points towards location of second mesio-buccal (MB2) canal. (B and C) Radiographs from disto-eccentric projection of maxillary first molar with four root filled canals, arrow points towards second mesio-buccal canal.
Molar teeth require some form of magnification to locate canal orifices, especially the second mesio-buccal canal (MB2) (category B) (figures 6 A-C). Teeth with anatomical variations ought to be treated by DP in category D (figure 2A and 7A-D).
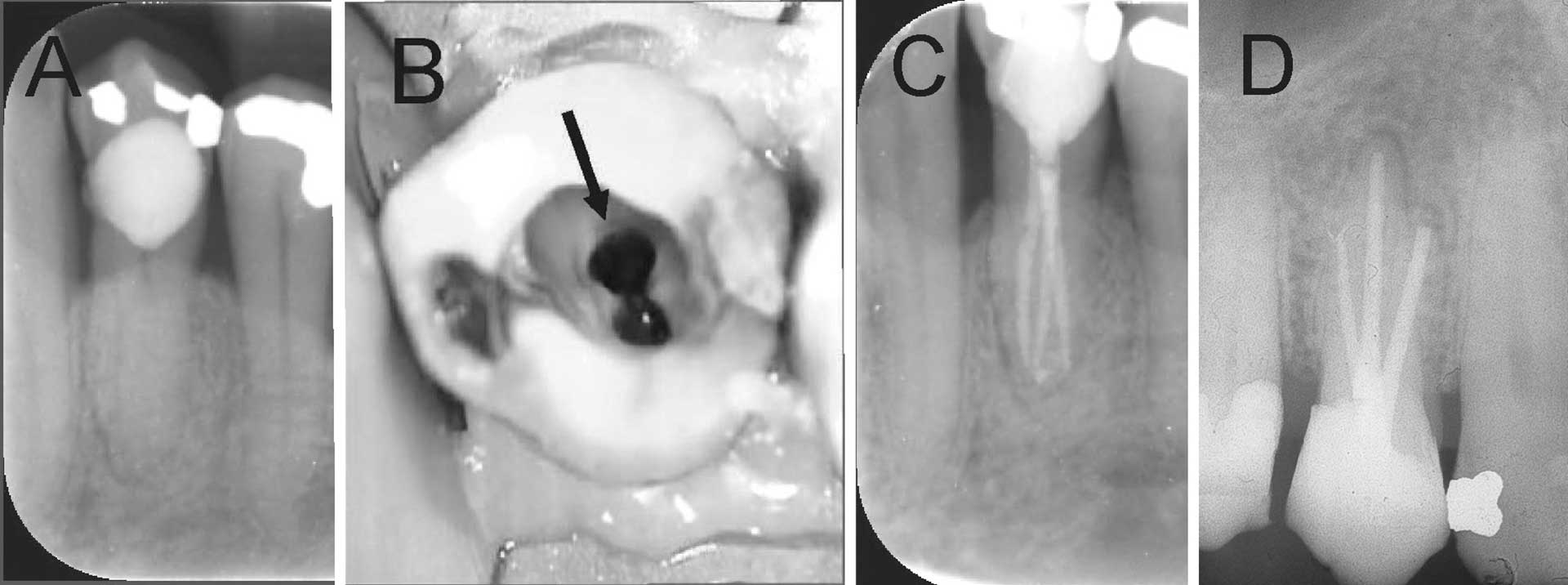
Figure 7. Mandibular right first premolar with anatomic variations and a large cervical restoration. (A) Radiograph shows root canal becomes indistinct just below the bone level (B) Clinical photo showing two buccal canal (arrow) and one lingual canal. (C) Final radiograph showing three root filled canals. (D) Radiograph of maxillary first premolar with three root canals.
Tooth inclination and rotation
A dentist in category A has not acquired adequate skills to modify cavity preparation in a tooth that is inclined or rotated. In order to avoid unnecessary mishaps, such as perforation during cavity preparation (figure 8A-F), these teeth ought to be treated by at category B DP.
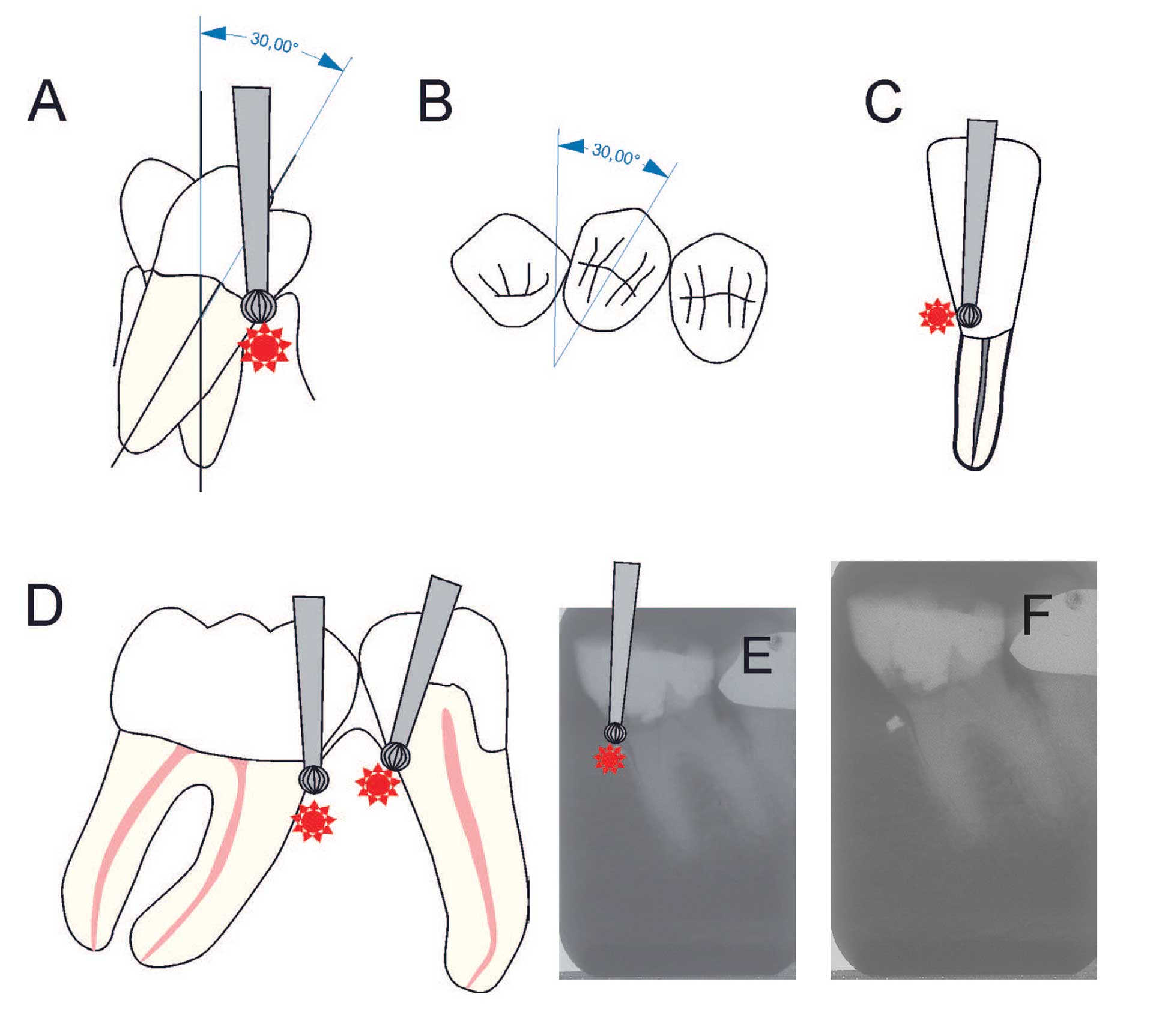
Figure 8. Schematic illustration of (A) a premolar with 300 lingual tilt [18]. Bur showing potential area of perforation (B) premolar with a 300 rotation (C) lower incisor with a mild/moderate tilt in the root but an over-contoured crown. Bur showing potential area of perforation. (D) premolar with distal tilt and molar with mesial tilt. Bur showing potential area of perforations [18]. (E) Radiograph showing a molar with a mild to moderate mesial tilt with bur showing area of perforation. (F) Radiograph of tooth with mesially placed access cavity preparation and foreign material lodged in the alveolar bone due to perforation.
Crown morphology
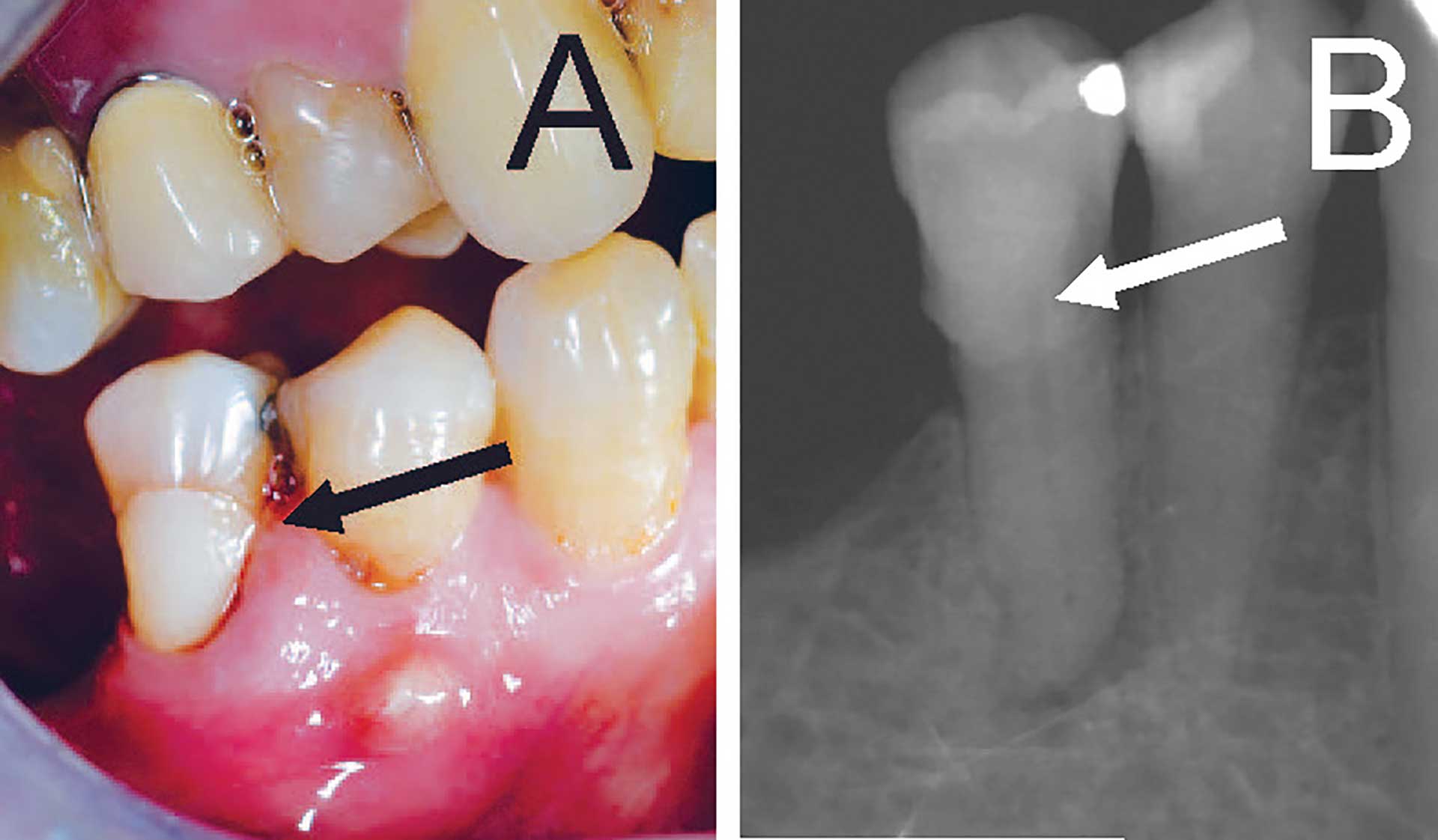
Figure 9. (A) Clinical photo of second premolar with large buccal cervical restoration (arrow) and fistula on buccal mucosa below first premolar. (B) Radiograph showing restoration in the coronal part (arrow) and periapical lesion under second premolar.
A severely broken-down tooth or restorations that do not reflect the original morphology of tooth lack original crown morphology for cavity preparation which can be difficult for a category A DP (figure 4). Teeth with deep cervical restorations are placed in category B (figures 9A and B) Teeth with full coverage crown and bridge abutment need careful preoperative assessment of radiographs (category C). Over-contoured or bulbous full coverage crowns are difficult to treat because of lack of orientation from original crown morphology (figure 10A). Teeth with ‘long’ crown length is difficult since cavity preparation needs to be extended deeper before canals are localized (category D) (figure 10B).
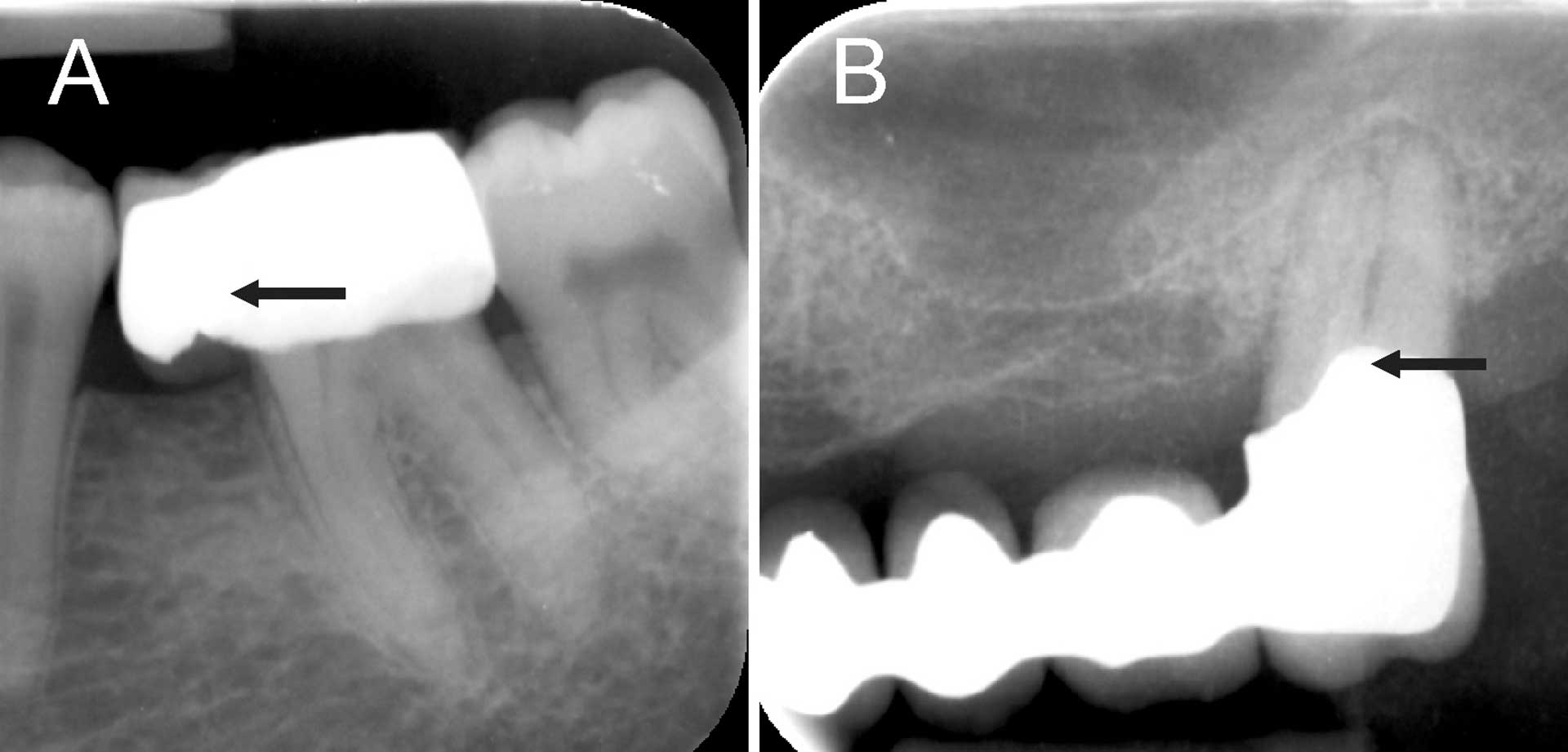
Figure 10. Radiograph of (A) mandibular second molar with full coverage crown that is over-contoured (arrow). (B) Maxillary second molar with a crown extending to furcation region (arrow) creating difficulty in assessing location of the pulp chamber.
Radiographic appearance
The presence of pulp stones in the pulp chamber can block canal orifices and therefore adequate magnification aids are necessary to locate canal orifices (category B) (figures 11A-C). A canal that is reduced in size needs more technical skills to negotiate a file to working length (category C).
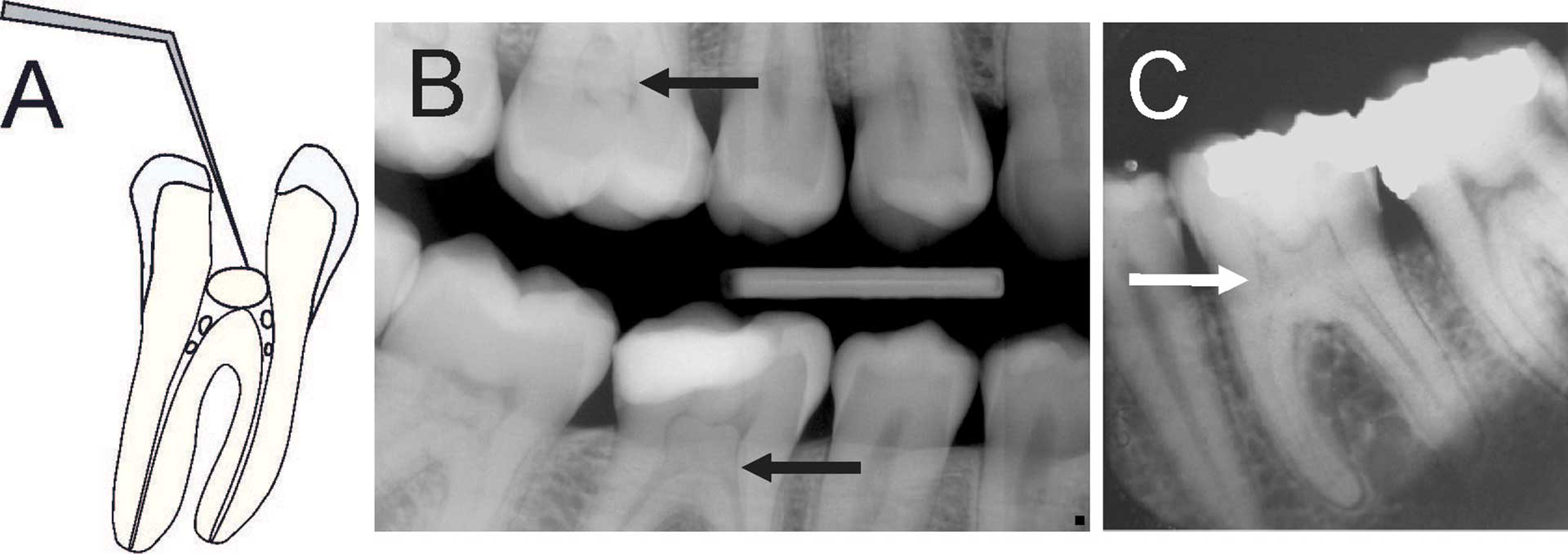
Figure 11. (A) Schematic illustration showing tooth with pulp stone in the chamber and root canals creating potential difficulty in locating root canal orifices and instrumentation [18] (B) Bitewing radiograph showing generalized pulp stone formation on molars (arrows). (C) Periapical radiograph of mandibular left first molar with extensive calcifications in the pulp chamber and root canals (arrow).
Root length and curvature
Teeth with long roots especially on molars are difficult to instrument (category B). Instrumentation of curved root canals can lead to mishaps such as instrument separation, ledge or zip formation, straightening of canal, lateral perforation or strip perforation. Therefore, teeth with curved canals (> 30° curvature) ought to be treated by at least category B DP (figure 12A-D) [22].
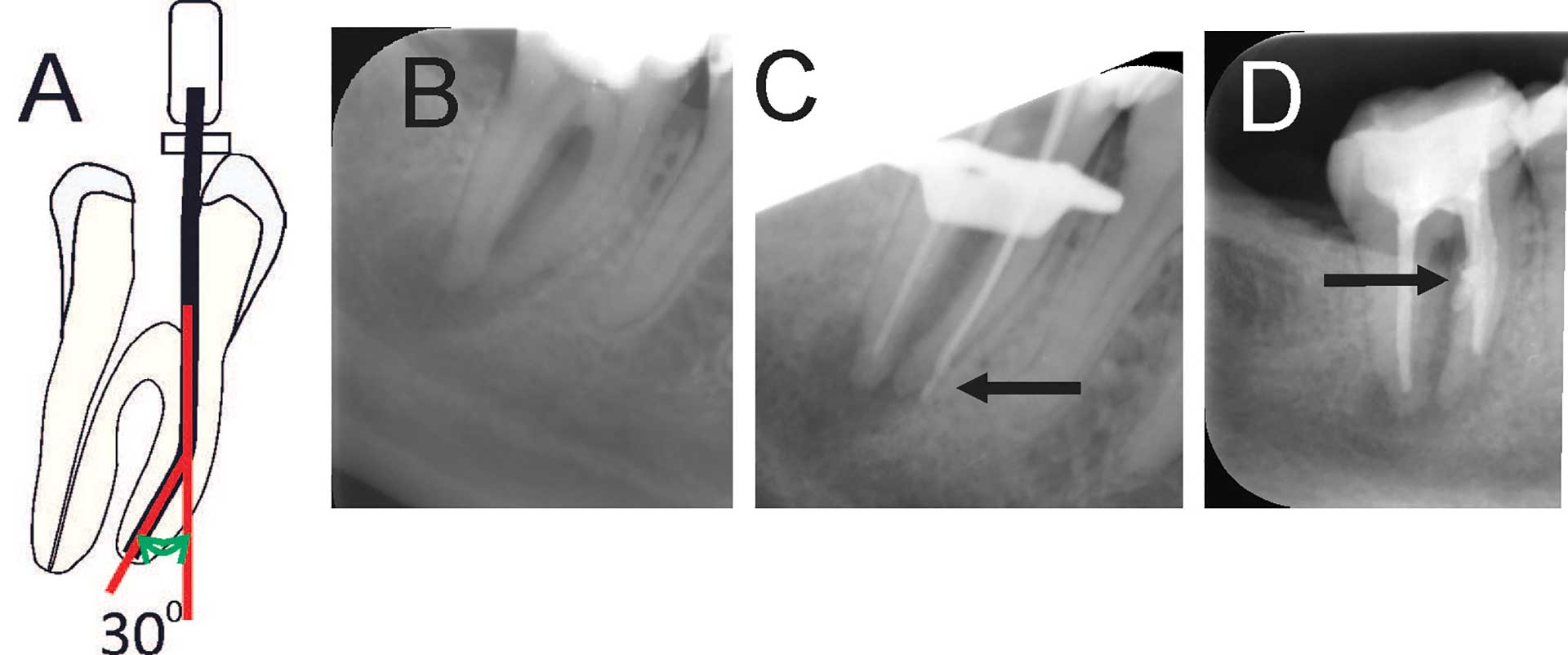
Figure 12. (A) Schematic illustration of 300 curvature on a root [18][21]. A root with more than 300 curvature is in category C. (B) Radiograph of mandibular second molar with more than 300 curvature. (C) Master point radiograph showing lateral perforation in the apical third of root canal (arrow). (D) Radiograph showing a strip perforation on the mesial root (arrow).
Dental trauma
Traumatic dental injuries often affect young individuals and require urgent care. Time and knowledge must be available to perform proper care initially. Correct diagnosis is of utmost importance for treatment strategy and proper care. Despite optimal care, one can expect a future need of endodontic treatment as the pulp can suffer damage from the traumatic injury [23][24] (figure 13A-C, 14A-C). Although young, undeveloped teeth is more resistant to pulp necrosis after traumatic injuries due to the good blood supply, these young teeth, in case of pulp necrosis, provides a technical treatment problem that requires good clinical knowledge and access to modern technology and materials for an optimal treatment result [25].
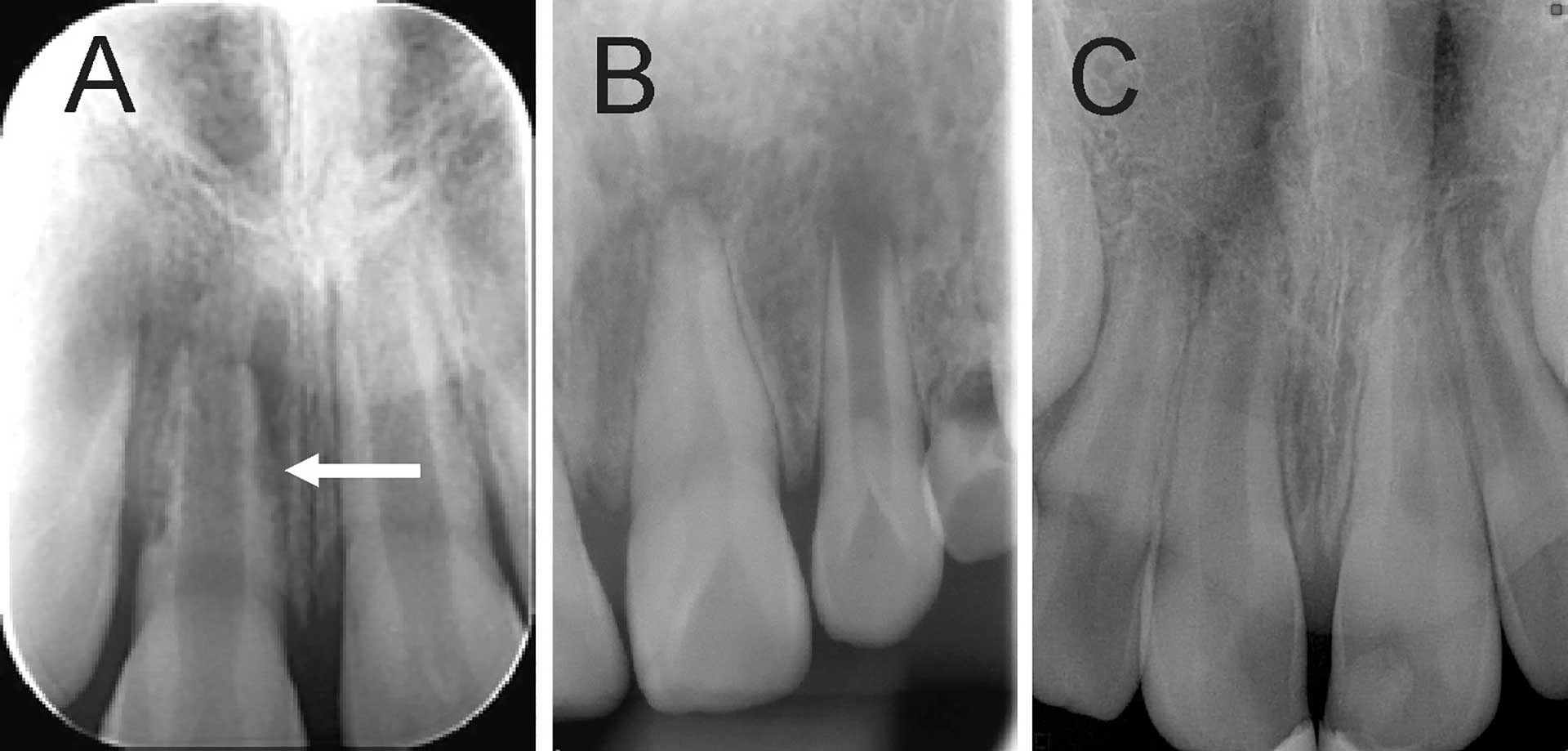
Figure 13. Radiograph of an immature permanent tooth after traumatic injury. (A) displaying root resorption on maxillary right central incisor (arrow). (B) Incomplete root development. (C) Periapical lesion on maxillary right central incisor and pulp calcification and root resorption on left central incisor.
The risk of necrosis after a luxation injury increases with the severity of the injury and is greatest for teeth with a complete root formation [26]. In the event of luxation injury, the patient should be followed up according to the guidelines developed by the Dental Trauma Guide [27]. Luxated teeth can present several different endodontic complications and proper treatment is crucial for the long-term survival of the tooth [28][29]. During follow-up, the injured tooth should be examined both clinically and radiographically and all signs of pathology must be considered (for example necrosis, obliterations and inflammatory/replacement resorptions).
It is often young individuals who suffer trauma injuries. It is therefore extremely important that these teeth are treated adequately as extraction in the young dentition often gives rise to difficulties regarding prosthetic replacement, especially in the aesthetic zone.
Root resorption
Root resorption (RR) is the loss of hard dental tissue (dentine and cementum) as a result of osteoclastic activity causing irreversible damage, and outcome can be unfavorable despite a combination of different treatment regimes. Pathological RR is classified as internal and external based on the site of the lesion. The use of Cone Beam CT for diagnosis has made it easier to diagnose RR and treatment plan (figure 14A-C). Although a majority of external RR occurs on a single tooth, a small proportion of patients present with multiple RR (figure 14D and E). Due to the difficulties of treating teeth with RR, it is placed in Category D.
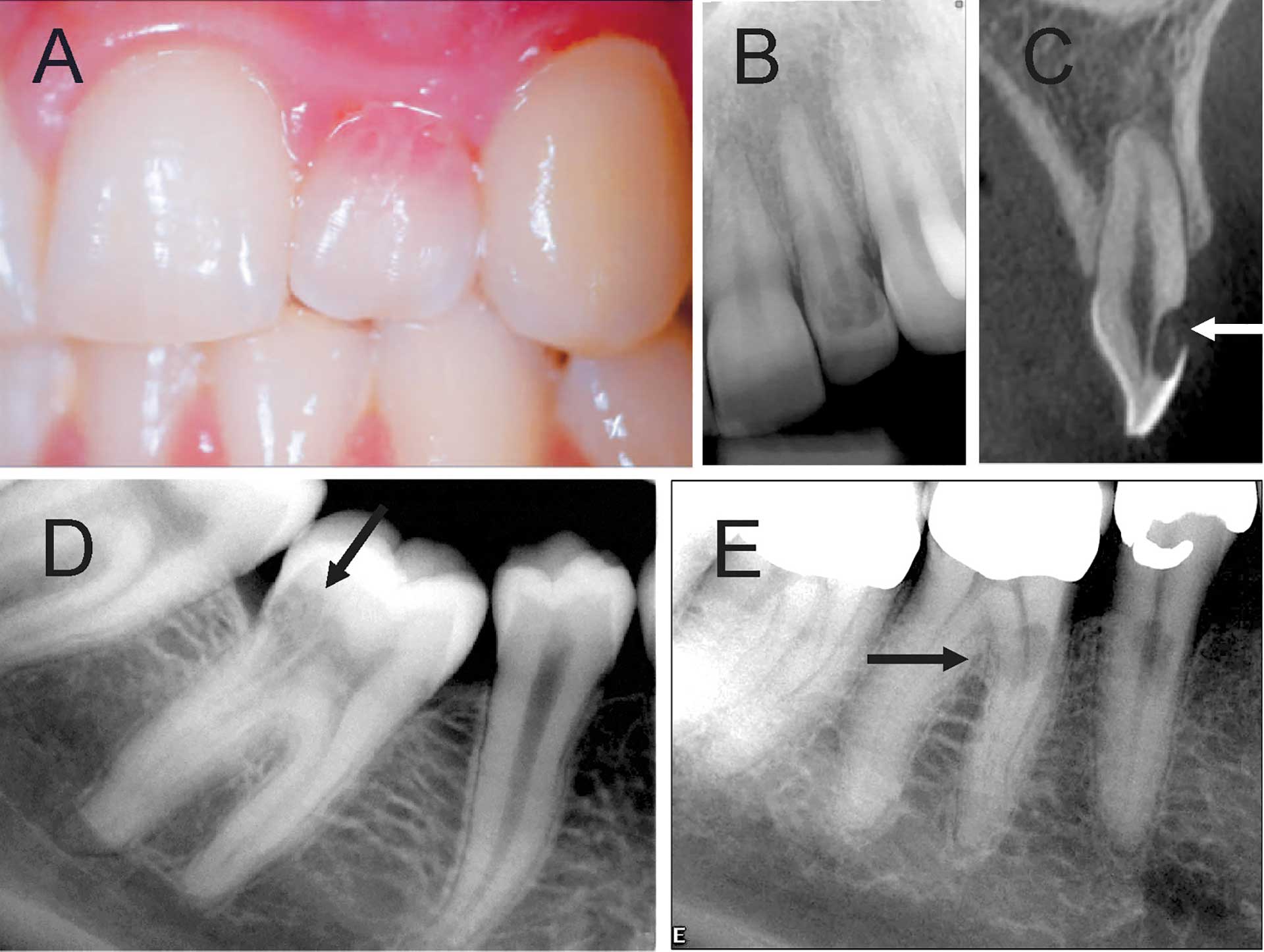
Figure 14. Root resorption. (A) Clinical photo showing a maxillary lateral incisor with a pink spot on the cervical part of the crown. (B) Radiograph showing resorption in coronal part of the tooth. (C) CBCT image showing a well circumscribed root resorption on labial surface (arrow) of the crown. (D) Cervical invasive root resorption on mandibular right first molar (arrow). (E) External root resorption on mandibular right second premolar and mesial root of first molar (arrow).
Health records
It has been observed that the quality of endodontic record keeping is not always adequate, and thus need for improvement is warranted [30]. Poor patient documentation in endodontics has been associated with the dentist’s male gender and higher age [31]. A detailed list of information that should be recorded for endodontic treatment is summarized in the consensus report of the European Society of Endodontology [32]. Key points in treatment records are previous symptoms, history of the tooth, results of clinical examination and sensitivity tests, report on radiographs, diagnosis, treatment plan, informed consent and details of the treatment protocol. Recommended radiographs include preoperative, working length determination if not measured electronically, and verification of the completed root canal preparation by taking a masterpoint and postoperative. Assessment of the treatment outcome by clinical and radiographic follow-up is recommended with a minimum observation period of 1 year.
When and how to refer
Communication with patients
To make a referral, good communication with the patient is essential. The patient needs to be informed why he/she is being referred to a specialist and what to expect, but not promising too much, for example assuming that removing a separated file is always easy or even possible. The cost of treatment should be disclosed, as well as prognosis and duration of treatment. If there has been an endodontic mishap such as a perforation or file separation, the patient needs to be informed (figure 15A-C). Post-treatment restoration, additional cost associated with restoration and who will be performing that treatment needs to be clearly indicated to the patient.
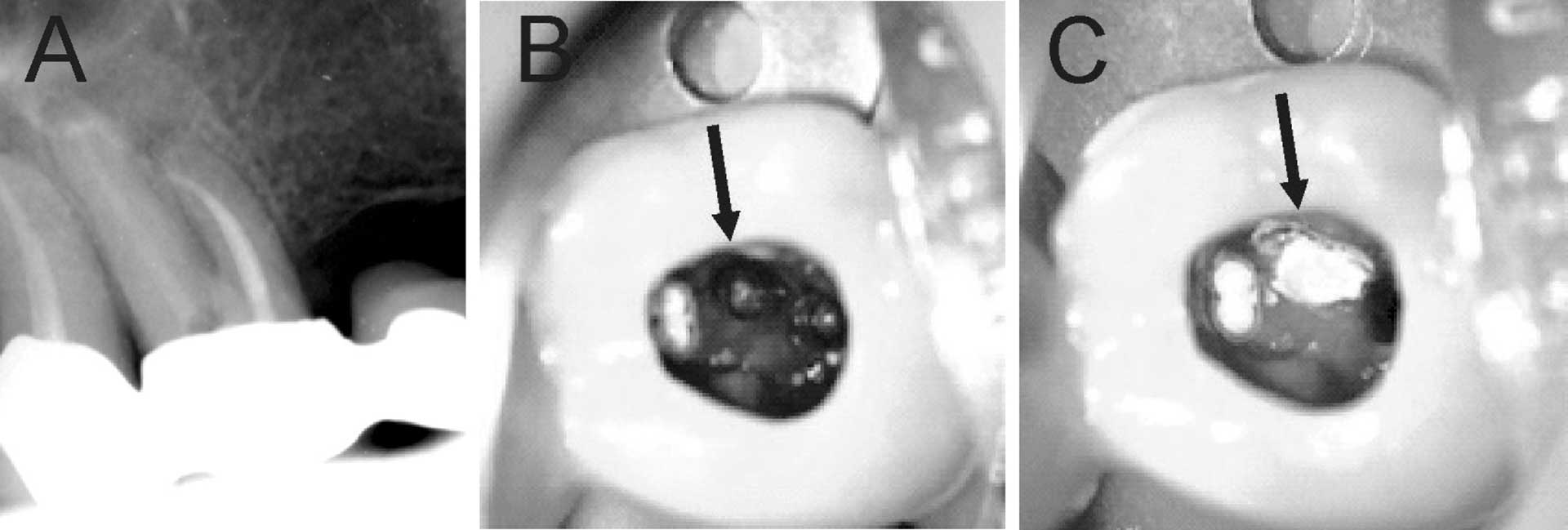
Figure 15. Patient was advised (with no referral) to continue treatment at the University Dental Clinic. First maxillary molar had root canal treatment initiated by private practitioner. (A) Preoperative radiograph showing root filled mesio-buccal canal. (B) Clinical photo after removal of temporary restoration showing root filled MB1 and MB2 canals, furcation perforation (arrow), instrumented disto-buccal canal and uninstrumented/unlocated palatal canal. (C) Furcation perforation was repaired (arrow), palatal canal located and instrumented.
Referral for treatment
The referral needs to be done early in the treatment procedure. Ideally let the Endodontist initiate the treatment. If there is a need for emergency treatment, perform minimally invasive treatment to help patient be symptom free. It is also good practice to contact the specialist and inquire if they can perform the emergency treatment. Instrumentation of a root canal without knowing the working length can lead to overinstrumentation or ledge formation. When diagnosis is uncertain, do not treat. Write a brief synopsis of the patient and tooth anamnesis, history of previous treatment, findings from clinical and radiographic examination. Write down the diagnosis or if uncertain, request for a diagnosis. A good quality radiograph should be provided. If relevant, a clear description of treatment already provided should also be included. Information of possible technical problems (missing canals, ledges, fractured files, perforations etc.) should be disclosed. Other patient related issues should be disclosed such as insurance details, dental anxiety, travel plans etc.
What to expect
After the treatment is completed, the specialist should communicate with the referring dentist and provide information on the treatment provided and its prognosis, a time frame for the next step and recall plan. If there is a need for a follow-up for example with apical surgery, this needs to be communicated to the referring DP. Copies of the pre- and postoperative radiographs are also made available.
Conclusions
In conclusion, to perform RCT on a tooth that is beyond one’s level of competence and without adequate tools and knowledge is far from standard of care. Endodontics is the leading cause in malpractice cases. Patients want to retain their natural teeth for their entire lifetime. Endodontically treated tooth needs to last a lifetime and therefore has to be done with precision the first time around. A good knowledge of case difficulty and operator abilities can help DP decide on whether they want to treat a tooth or refer to a specialist.
References
Haug SR, Solfjeld AF, Ranheim LE, Bårdsen A. Impact of Case Difficulty on Endodontic Mishaps in an Undergraduate Student Clinic. J Endod. 2018;44(7):1088-95.
Alnæs M, Guttormsen AB, Björkman L. Fatal anafylaksi etter tannbehandling. Nor Tannlegeforen Tid. 2021;131:472-3.
Alnæs M, Storaas T, Björkman, L, Vindenes HK, Brudevoll S. Anafylaksi etter endodontisk behandling. Nor Tannlegeforen Tid. 2020;130:326-30.
Givol N, Rosen E, Taicher S, Tsesis I. Risk management in endodontics. J Endod. 2010;36(6):982-4.
Farook SA, Shah V, Lenouvel D, Sheikh O, Sadiq Z, Cascarini L, et al. Guidelines for management of sodium hypochlorite extrusion injuries. Br Dent J. 2014;217(12):679-84.
Swanljung O, Vehkalahti MM. Root Canal Irrigants and Medicaments in Endodontic Malpractice Cases: A Nationwide Longitudinal Observation. J Endod. 2018;44(4):559-64.
Walton RE, Torabinejad M. Principles and Practice of Endodontics: Saunders; 2002.
Mohammadi Z, Shalavi S, Jafarzadeh H. Extra roots and root canals in premolar and molar teeth: review of an endodontic challenge. J Contemp Dent Pract. 2013;14(5):980-6.
Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58(5):589-99.
Costa F, Pacheco-Yanes J, Siqueira JF, Jr., Oliveira ACS, Gazzaneo I, Amorim CA, et al. Association between missed canals and apical periodontitis. Int Endod J. 2019;52(4):400-6.
Vehkalahti MM, Swanljung O. Accidental perforations during root canal treatment: an 8-year nationwide perspective on healthcare malpractice claims. Clin Oral Investig. 2020;24(10):3683-90.
Ungerechts C, Bårdsen A, Fristad I. Instrument fracture in root canals - where, why, when and what? A study from a student clinic. Int Endod J. 2014;47(2):183-90.
Suter B, Lussi A, Sequeira P. Probability of removing fractured instruments from root canals. Int Endod J. 2005;38(2):112-23.
Sjögren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.
Shakiba B, Hamedy R, Pak JG, Barbizam JV, Ogawa R, White SN. Influence of increased patient age on longitudinal outcomes of root canal treatment: a systematic review. Gerodontology. 2017;34(1):101-9.
Zilinskaite-Petrauskiene I, Haug SR. A Comparison of Endodontic Treatment Factors, Operator Difficulties, and Perceived Oral Health-related Quality of Life between Elderly and Young Patients. J Endod. 2021;47(12):1844-53.
Kiefner P, Connert T, ElAyouti A, Weiger R. Treatment of calcified root canals in elderly people: a clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology. 2017;34(2):164-70.
Haug SR. Preoperativ kasusvurdering i endodonti. Nor Tannlegeforen Tid. 2021;131:464-71.
American Association of Endodontists. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/educatorguidetocdaf.pdf 2017.
Haug SR, Linde BR, Christensen HQ, Vilhjalmsson VH, Bårdsen A. An investigation into security, self-confidence and gender differences related to undergraduate education in Endodontics. Int Endod J. 2021;54(5):802-11.
Christensen HQ, Linde BR., Bårdsen A, Vilhjalmsson VH, Haug SR. Influence of dental education on adoption and integration of technological aids in the delivery of endodontic care by dental practitioners: A survey, Acta Odontol Scand. 2022. DOI: 10.1080/00016357.2022.2071986
Schneider SW. A comparison of canal preparations in straight and curved root canals. Oral Surg Oral Med Oral Pathol. 1971;32(2):271-5.
Andreasen FM, Kahler B. Pulpal response after acute dental injury in the permanent dentition: clinical implications-a review. J Endod. 2015;41(3):299-308.
Wang C, Qin M, Guan Y. Analysis of pulp prognosis in 603 permanent teeth with uncomplicated crown fracture with or without luxation. Dent Traumatol. 2014;30(5):333-7.
Sivertsen TB, Vilhjálmsson VH, Fristad I, Bårdsen A, Haug SR. Endodontisk behandling av umodne permanente tenner. Nor Tannlegeforen Tid. 2013;123:198-201.
Andreasen FM, Zhijie Y, Thomsen BL. Relationship between pulp dimensions and development of pulp necrosis after luxation injuries in the permanent dentition. Endod Dent Traumatol. 1986;2(3):90-8.
Dental Trauma Guide. https://dentaltraumaguide.org.
Robertson A, Andreasen FM, Andreasen JO, Noren JG. Long-term prognosis of crown-fractured permanent incisors. The effect of stage of root development and associated luxation injury. Int J Paediatr Dent. 2000;10(3):191-9.
Soares AJ, Souza GA, Pereira AC, Vargas-Neto J, Zaia AA, Silva EJ. Frequency of root resorption following trauma to permanent teeth. J Oral Sci. 2015;57(2):73-8.
King E, Shekaran L, Muthukrishnan A. Improving the quality of endodontic record keeping through clinical audit. Br Dent J. 2017;222(5):373-80.
Vehkalahti MM, Swanljung O. Operator-related aspects in endodontic malpractice claims in Finland. Acta Odontol Scand. 2017;75(3):155-60.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. International Endodontic Journal. 2006;39(12):921-30.
Corresponding author: Sivakami Rethnam Haug. E-mail: Sivakami.Haug@uib.no
Accepted for publication 06.08.2022
The article is peer reviewed.
Haug SR, Siukosaari P, Furuholm J, Brundin M. An evaluation of case difficulty, operator abilities, when and how to refer. Nor Tannlegeforen Tid. 2023; 133:
Keywords: Nordic Endodontic Assessment Form; Health records; Referral
