Uncertainties and decision making in endodontics
Headline
This paper is concerned with uncertainties and decision making in endodontics. Uncertainties are of different kinds; risk, fundamental uncertainty, ignorance and indeterminacy. The various types of uncertainties that are involved in the process of clinical making decisions are briefly reviewed in case of an injured vital pulp, a necrotic pulp with apical periodontitis and finally a root-filled tooth with a persistent apical lesion.
Professional judgments in endodontics as in any medical discipline must be based on qualified estimations of the probability and value of relevant outcomes. In this paper, we briefly discuss how attention to various types of uncertainties are involved in the most common endodontic decision-making situations.
Uncertainty
There are many kinds of uncertainties that are relevant to decision-making in endodontics [1] [2]. First there are situations where the outcomes are well known, and we know the probability distributions of these outcomes. That is, we know what might happen, and we know the probability that it will happen. For example, we know that some vital teeth will become necrotic following crown preparation and we know its probability distribution. This is frequently referred to as risk. However, oftentimes we know the outcomes, i.e., what might happen, but we do not know the probability distributions. This is called fundamental uncertainty. This, of course, makes it more difficult to make decisions, and we try to reduce fundamental uncertainty to risk by expanding evidence. However, we may also encounter situations where we do not know the outcomes. That is, unexpected things may happen. This is called ignorance in philosophy of science as in ordinary language. For good and bad, we need to be aware of such unexpected outcomes. As with the discovery of X-rays, unexpected consequences can be beneficial. However, they can also be detrimental. One additional kind of uncertainty is not related to knowledge of outcomes and their probability distributions. It is related to how we define things. Pulpitis can be defined and classified in different ways, and presence of apical periodontitis, particularly in connection with root filled teeth, can be determined in a variety of ways. Which definitions and measures we apply may depend on what we want to obtain, i.e., our social commitments. This type of uncertainty is frequently called indeterminacy. Hence, when we make decisions, it is crucial that we base them on evidence that applies definitions and measures that are relevant to the specific case that we are treating. In sum, we face with four types of uncertainty that are relevant for decision-making: risk, fundamentaluncertainty, ignorance, and indeterminacy.
Decision making
When practicing, the dentist constantly makes a lot of decisions of various kinds. The term “clinical decision making” usually refers to the management of three fundamental questions. “What is the problem?”, “What are the possible solutions?” and “What is the best solution for this patient”? [3]. Clinical decision-making can be examined from both a descriptive and normative approach. Descriptive projects aim at mapping out and explaining clinicians’ reasoning and how they make decisions. Normative projects, on the other hand, are involved with how decisions should or ought to be made.
Descriptive decision making
Several models have been suggested to describe how clinicians make decisions [4]. Some investigators have concentrated on the artistic, or intuitive, aspects of clinical practice [5] [6]. Using “judgement analysis” researchers have tried to reveal the pieces of information or “cues”, used at conscious or unconscious levels, that effect a person’s decision-making [7]. In a series of investigations Tversky & Kahneman explored the idea that people most often rely on a small number of heuristic principles to make decisions. Their important empiric supported insights into human thinking have been summarized in an easy-to-read bestseller [8].
Normative decision making
There is no general agreement of the right way to make decisions clinical decisions. Dentistry, like medicine, is an applied science. Since each patient is unique and have distinctive preferences, it can be tricky to decide how to apply the science and evidence to each individual situation. Each clinician compiles their own data and constructs an argument based on their interpretation of “facts”. The strength of their case will depend on the way they collect and interpret information [9]. The patient’s participation in the process is central. Autonomy, or self-determination, means that an individual has the right to decide on matters regarding his/her own body, mind and life. The right to autonomy has a strong foundation in diverse ethical theories [10] and includes a person’s right to decide on his/her health care. To be able to make an autonomous decision, the dentist consequently must to the best of his/ her ability provide the patient with all relevant facts; the findings, the etiology of the disorder, the various possible options to deal with the situation, risks, and probable long-term outcome with or without any treatment. The clinician must also be able to discern the essential circumstances that characterize the specific situation and needs. A two-way communication of shared information and decision-making should always precede a medical decision whether to treat or not. At the center is the patient’s right to accept or decline treatment suggested by a clinician, be it detrimental or beneficial. There are some core skills that the professional needs to acquire to make good decisions as often as possible (Key box 1).
Key box 1
The core skills of a professional practitioner.
Evidence awareness.
Being up-to-date with best available evidence and practice guidelines.Communication competence.
Listening to patients’ experiences, values, and preferences and to be able to communicate information in a comprehensible way.Clinical experience.
Gathering years of experience in clinical practice and learning to recognize patterns. Sharing experience with and learning from colleagues.Critical thinking.
Recognizing emotions, personal attitudes, and bias in reasoning and assumptions.Self-reflection.
Using feed-back from others and the outcomes of previous decisions to consider possible future improvements.
Clinical decision analysis
The theoretical framework of clinical decision analysis is based on “expected utility theory” [11]. The model was introduced to medicine by Ledley & Lusted [12] and has received much attention in medicine but less so in dentistry.
According to its proponents, a decision problem should be structured into a “decision-tree”, which (i) logically displays available actions and their possible consequences. Then (ii) the listed outcomes are assessed regarding probabilities and subjective values (“utility”). After this (iii) the weighed sum (expected utility) of each strategy is computed, and (iv) the action with the highest sum is chosen.
Within endodontics, a decision analysis approach has been applied for example to the selection of treatment strategies in teeth with apical periodontitis [13], direct pulp capping procedures [14].
Even though the validity and usefulness of decision analysis has been questioned as a normative model for making clinical decisions, it benefits from pointing out two equally essential components: empirical facts and subjective values of the patients or other stakeholders. Moreover, the model includes one type of uncertainty, i.e., risk. Additionally, the expected utility may be subject to indeterminacy.
Decision-making in endodontics
As listed in Key box 2, within the context of clinical endodontic decision making mainly correspond to one of three conditions regarding a particular tooth. An overview of clinical endodontic decision-making is illustrated in Figure 1.
Key box 2
Three common endodontic decision-making situations.
In case of a decayed or injured tooth - How severely damaged is the pulp? What are the options if the pulp is still vital? What are the advantages and disadvantages of keeping the pulp vital in this case?
In case of a tooth with a suspected necrotic pulp and apical periodontitis - How should pulp necrosis and AP be confirmed or rejected? If the pulp is necrotic, is the root canal treatment or extraction preferable to this tooth and this patient?
In case of an asymptomatic root-filled tooth but with radiographical signs of non-healing apical periodontitis - Does the condition (tooth; patient) need attention, monitoring or treatment? If yes, what is the best treatment option; retreatment, surgical intervention, or extraction?
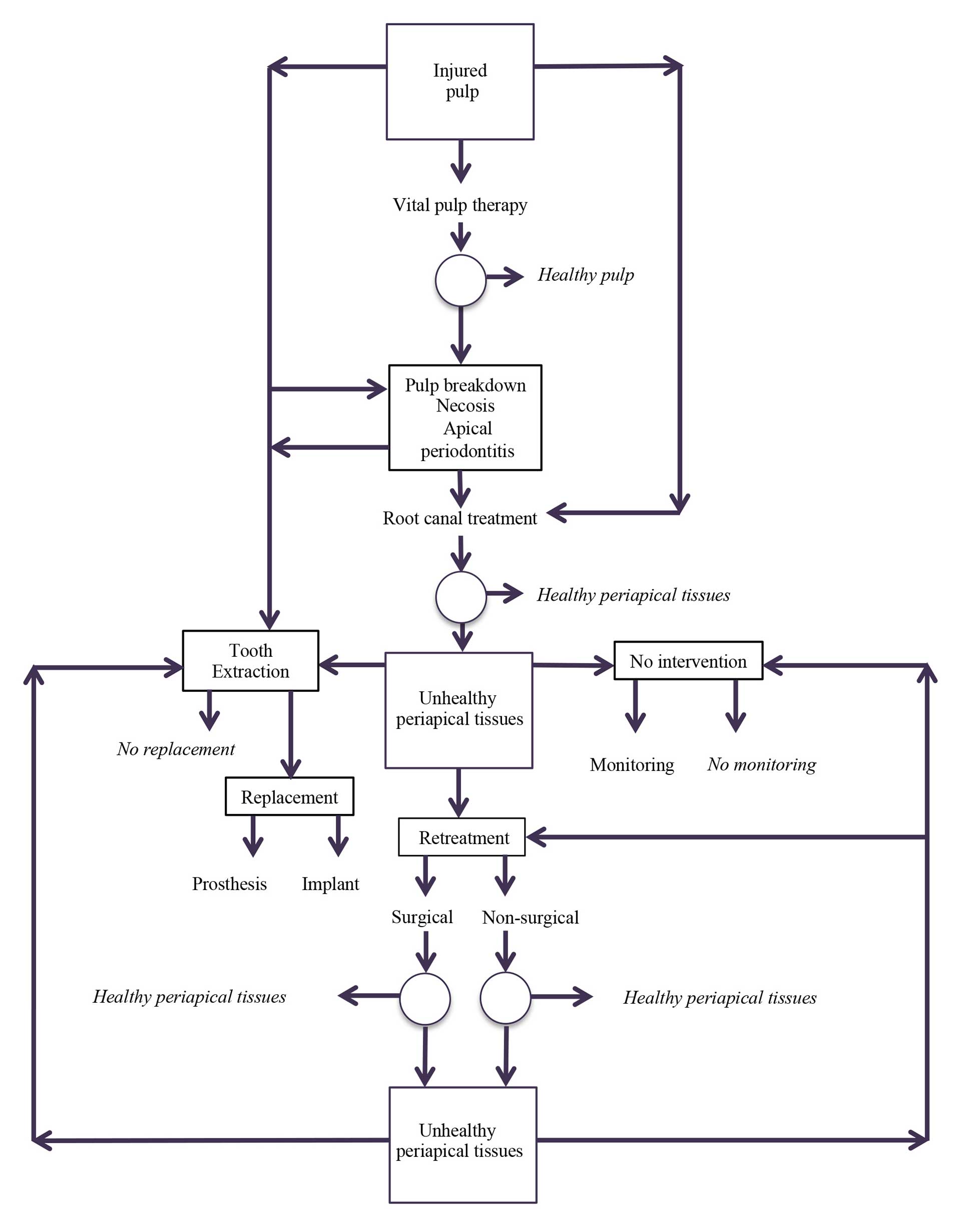
Figure 1. Decision making in endodontics at a glance. In the squares, there are conditions or situations where a clinical decision needs to be made. The circles represent uncertainty after a decision and action. Conditions in italics represent final outcomes where no further clinical decisions need to be made. The other end-points may require further decision making
Decision making in case of an injured but vital dental pulp
The uncertainty in determining the pulp’s potential to heal
Vital pulp treatment can be defined as “strategies aimed at maintaining the health of all or part of the pulp” [15]. The ultimate aim is to avoid an unnecessarily invasive procedure, root canal treatment, which is more costly, more time-consuming and associated with the risks of complications, including the development of apical periodontitis. Which, all in all, increases the risk of tooth loss. The success of vital pulp treatment depends on the type of treatment and on the inflammatory state of the pulp. For example, the success rate for partial pulpotomy can vary from over 95% in young teeth where the pulp was exposed by trauma [16] to under 40% in mature teeth where the pulp was exposed by deep caries and the tooth had a history of pain [17]. For teeth with pulp exposure due to trauma, a vital pulp treatment (direct pulp capping or partial pulpotomy) to maintain the vitality of the tooth is generally recommended as a first choice [18].
When the pulp is exposed due to caries the decision making remains controversial. Traditionally, the pulp state has been classified into reversible and irreversible pulpitis. It was thought that the pulp vitality could only be maintained in teeth where the pulp state was classified as reversible pulpitis. Methods to determine the level of pulp inflammation into a reversible or irreversible state have been through anamnesis (history of pain), clinical tests and radiographic examination. Clinical indicators that have been linked to treatment failure after vital pulp treatment are conspicuous bleeding from the pulp on exposure [19] and extremely deep caries [20]. Unfortunately, there is not enough evidence that a treatable pulpitis can be distinguished from non-treatable pulpitis with the methods so far used to assess the level of pulp inflammation [21]. The use of the terms “reversible” versus “irreversible” pulpitis thus is an example of indeterminacy since these terms consciously or unconsciously may control the clinician’s choice of treatment. Focus on minimally invasive techniques, antiseptic protocols and new materials has aroused interest in the possibility of successful vital pulp treatments in teeth with signs and symptoms previously considered to be significative of irreversible inflammation [22]. In teeth with pulp exposure due to caries some studies have demonstrated a better prognosis for vital pulp treatment with tricalcium silicate cements compared to calcium hydroxide [23]. The efforts to find evidence for pulp survival probability is an example of reducing fundamental uncertainty to risk.
Weighing the advantages and disadvantages of saving the pulp
The advantages with vital pulp treatments are their minimally invasive approach, retaining healthy pulp and preventing apical periodontitis [19]. Health economic evaluations indicate that pulp capping is a cost-effective alternative to root canal treatment in adults under the age of 50 with occlusal caries pulp exposures [24], and in permanent teeth in children and adolescents [25]. Retrospective studies indicate a poor outcome of root canal treatment in children and adolescents. In one retrospective study apical periodontitis was found in 52% of the root filled teeth [26], and another study estimated the 5-year pulp survival probability to lower than 50% for root filled teeth in children aged 6-11 [27].
However, both in children and adults the advantages with vital pulp treatment in teeth with pulp exposure due to caries must also be weighed against the risk for pain. In one study, the majority of patients in whom the pulp capping or partial pulpotomy failed, it was because they developed intensely painful symptoms [17].
Decision making in a necrotic tooth with apical periodontitis
Clinical decision regarding the treatment of a tooth with a necrotic pulp with apical periodontitis requires thorough consideration. Root canal treatment is the only option to conserve the tooth and at the same time establish healthy periradicular tissues. In addition to the mere evaluation of the endodontic conditions of the tooth, the dentist also has to evaluate the patient’s general and oral health condition, his or her preferences and compliance and the practicality of restoring the tooth. Also, the costs need to be evaluated against the potential benefits and harms, and comparing alternative options, i.e., extraction with or without replacement. The issues involved in the decision making can be summarized in three cornerstones: the patient, the tooth, and the overall prognosis. The clinical questions that need to considered before starting a root canal treatment are listed in Key box 3.
Key box 3
Clinical questions of importance to the dentist as well as the patient before deciding on starting root canal treatment of a tooth with necrotic pulp and apical periodontitis.
Is tooth survival beneficial for the patient’s general health?
Is the tooth functionally and aesthetically strategic?
What is the patient’s attitude towards the condition and root canal treatment?
Is the tooth possible to isolate and to restore?
What is the prognosis of root canal treatment in terms tooth survival, tooth comfort and healing periapical tissues?
The role of systemic disease in relation to decision making of teeth with apical periodontitis and root canal treatment is not obvious. For example, in diabetic patients the healing of the periapical disease is significantly slower or impaired [28]. In case the root canal infection cannot be eliminated or at least greatly reduced, the risk of local symptoms and adverse effects on the general health due to chronic periapical inflammation must be assessed [29]. On the other hand, saving teeth by root canal treatment may be beneficial for general health [30] while high frequency of lost teeth is associated with poorer general health [29] or even mortality [31]. The issue of the connection between endodontic inflammatory disease and various detrimental effects on systemic health are so far an example of fundamental uncertainty. We know that there are associations, but a lot of research remain to be done until we will know the risks.
Usually, the tooth requiring root canal treatment has lost much of the tooth structure and/or has already been extensively restored. Loss of coronal structure due to caries and cavity preparations inevitably reduce the tooth mechanical fracture strength, and loss of proximal walls creates a wedge effect. Adequate restoration of a root filled tooth is considered important for the long-term success both in relation to tooth survival as well as healing of the periradicular tissues [32].
Sufficient remaining tooth structure and maintaining cavity walls that allow the ferrule effect and indirect restorations with cuspal coverage in premolar-molar regions [32] are the predominant factors determining survival of endodontically treated teeth while positive effect of post has not been confirmed [33]. The last tooth in a row, especially those without proximal contacts, and increased periodontal probing depth associated with a crack increase the risk of failure [32]. Considering all these factors, taking also into account the patient preferences, help the clinician to decide what are the chances of long-term success.
Root canal treatment, especially in molars, often involves extensive technical difficulties. The dentist’s skill, experience and facilities vary, and sometimes it is difficult to estimate the difficulty level before the initiation of the treatment. In any case, the dentist needs to consider whether the root canal treatment might be best performed by a specialist.
There’s a number of tools to aid in the endodontic case difficulty assessment, that allows the scoring of anamnestic, patient- and tooth-related conditions summing up to the total difficulty level. A recent tool is the Dental Practicality Index (DPI) [34], which takes into account also the practicality of the endodontic-restorative treatment. As the DPI score increases, more careful reflection of the alternative options is warranted [34].
Extraction and an implant is sometimes seen as an alternative to endodontic treatment. Regardless of a chosen approach, the aim is to build a good coronal structure: endodontic and restorative treatment or implant are only ways to get there. Before going for an implant, there are several aspects that may affect the prognosis of both endo and implant are worth of thought before choosing an implant over endodontic treatment [35]. Implants tend to require significantly more post-treatment interventions than endodontically treated teeth [36]. And root canal treatment is highly cost-effective compared to the implant as a first line intervention [37]. Sometimes, a fixed prostheses construction may be the best option that trumps both a root canal treatment and an implant [35]. The alternative of extracting a severely damaged tooth in need of root canal treatment and leaving the site without replacement can also sometimes be the best alternative, not least in the posterior molar region.
Decision making of a root filled tooth with apical periodontitis
Based on studies undertaken at universities, dental hospitals and specialist clinics, the expected healing rate of apical periodontitis following adequate root canal treatment is in the range of 85% - 96% [38].
However, in epidemiological studies the prevalence of persistent apical periodontitis in root filled teeth is 25%- 50% [39]. The majority of cases remain more or less asymptomatic over many years [40] and thus are diagnosed at a routine examination or as an incidental finding.
According to the prevailing academic paradigm, a root filled tooth with apical periodontitis is defined as an “endodontic failure” and thus implies a clinical decision and action [41] [42]. The repeatedly demonstrated variation in clinical decisions and in particular the reluctance among practitioners to institute retreatment has bothered scholars in endodontology since the 1980’s [43].
The sources of the variation fall into two main categories of disagreement; facts and values [44]. It is a fact that there is lack of solid scientific evidence for questions regarding both diagnosis of a “failure” and outcome of retreatment [21] [45]. That is, we lack knowledge about the probability distributions for all outcomes (fundamental uncertainty) and there may be outcomes that we have not taken into account (ignorance). In particular, few studies have reported the consequences regarding a conservative no-intervention alternative [39]. However, a lot of the variation stems from issues about different perceptions of disease, and values concerning the condition [45], i.e., to indeterminacy.
Summary and conclusion
As we have illustrated in this article, in many cases we know the outcomes and their probabilities, i.e., we know the risk. Informing patients about risk is not easy, as risk communication and perception can be biased. Handling risk is not easy for professionals either, as you do not know how this particular patient fits in the spectrum of available evidence and specifically what will happen with this particular patient. As we have illustrated, the evidence is not always clear as various studies may have diverging results. Hence, we have some indication of risk, but are not well informed about the probability distribution. However, we are on the move from fundamental uncertainty to risk. In this progress, knowledge elicited by good clinical research is of paramount importance. Meanwhile, we may arrange consensus conferences, protocols and statements making judgments based on the best available evidence, establishing professional paradigms. While these may serve as useful heuristics, it is crucial to maintain critical reflection on their validity and utility. Moreover, we must always try to be alert to the unexpected (ignorance) and to improve the definitions of our basic concepts, in order to reduce indeterminacy. We should refine and define the concepts in ways that make us best able to help patients with their pain and suffering, i.e., in alignment with our professional duties.
References
Hofmann B, Holm S. Philosophy of Science. In: Laake P, Benestad HB, Olsen BR, editors. Research in Medical and Biological Sciences: From Planning and Preparation of Grant Application and Publication: Academic Press; 2015:1-42.
Pigg M, Brodén J, Fransson H; EndoReCo; the Foresight Research Consortium, Vareman N. How do we and how should we deal with uncertainty in endodontics? Int Endod J. 2022; Online ahead of print. doi: 10.1111/iej.13679.
Pellegrino E, Thomasa D. A philosophical basis of medical practice: towards a philosophy and ethic of the healing professions. Oxford:Oxford University Press. 1980.
Dowie J, Elstein A. Professional judgement. A reader in clinical decision making. Cambridge, UK: Cambridge University Press. 1988.
Schön DA. The reflective practitioner: How professionals think in action. New York: Basic Books, Inc. Publishers. 1983.
Groopman J. How doctors think. Houghton Mifflin Co.: Boston, Massachusetts, USA. 2007.
Brehmer B, Brehmer B. What have we learned about human judgment from thirty years of policy capturing? In: Brehmer, CRB Joyce (Eds.), Human Judgment. The SJT view, Elsevier, Amsterdam (1988), pp. 75-114.
Kahneman D. Thinking, fast and slow. 1 ed. New York: Farrar, Straus and Giroux; London: Allen Lane, 2011.
Trimble M, Hamilton P. The thinking doctor: clinical decision making in contemporary medicine. Clin Med (London). 2016 Aug;16(4):343-6.
Beauchamp TL, Childress FF. Principles of Biomedical Ethics. 8th edn. 2019; New York, USA, Oxford University Press.
Von Neumann J, Morgenstern, O. Theory of games and economic behavior. 1947; Princeton university press. Princeton. USA.
Ledley RS, Lusted LB. Reasoning foundations of medical diagnosis. Science. 1959;130:9–21.
Reit C, Dahlén G. Decision making analysis of endodontic treatment strategies in teeth with apical periodontitis. Int Endod J. 1988;21:291-9.
Maryniuk GA, Haywood VB. Placement of cast restorations over direct pulp capping procedures: a decision analytic approach. J Am Dent Assoc. 1990;120:183-7.
European Society of Endodontology (ESE) developed by: Duncan HF, Galler KM, Tomson PL, Simon S, E-Karim I, Kundzina R, Krastl G, Dammaschke T, Fransson H, Markvart M, Zehnder M, Bjørndal L. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int Endod J. 2019;52:923-934.
Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1978;4:232-7.
Bjørndal L, Reit C, Bruun G, et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. European Journal of Oral Sciences. 2010;118:290-297.
European Society of Endodontology (ESE) developed by: Krastl G, Weiger R, Filippi A, Van Waes H, Ebeleseder K, Ree M, Connert T, Widbiller M, Tjäderhane L, Dummer PMH, Galler K. European Society of Endodontology position statement: endodontic management of traumatized permanent teeth. Int Endod J. 2021;54:1473-1481.
Matsuo T, Nakanishi T, Shimizu H, Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod. 1996;22:551-6.
Careddu R, Duncan HF. A prospective clinical study investigating the effectiveness of partial pulpotomy after relating preoperative symptoms to a new and established classification of pulpitis. Int Endod J. 2021;54:2156-2172.
Swedish Council on Health Technology Assessment (2010) Rotfyllning–en systematisk litteraturöversikt (In Swedish), Swedish Council on Health Technology Assessment.Report 203, 2010. English translation, Methods of diagnosis and treatment in endodontics. Accessible at http://www.sbu.se).
Duncan HF. Present status and future directions-Vital pulp treatment and pulp preservation strategies. Int Endod J. 2022 Jan 26. doi: 10.1111/iej.13688. Epub ahead of print.
Cushley S, Duncan HF, Lappin MJ, Chua P, Elamin AD, Clarke M, El-Karim IA. Efficacy of direct pulp capping for management of cariously exposed pulps in permanent teeth: a systematic review and meta-analysis. Int Endod J. 2021;54:556-571.
Schwendicke F, Stolpe M. Direct pulp capping after a carious exposure versus root canal treatment: a cost-effectiveness analysis. J Endod. 2014;40:1764-70.
Brodén J, Davidson T, Fransson H. Cost-effectiveness of pulp capping and root canal treatment of young permanent teeth. Acta Odontol Scand. 2019;77:275-281.
Ridell K, Petersson A, Matsson L, Mejàre I. Periapical status and technical quality of root-filled teeth in Swedish adolescents and young adults. A retrospective study. Acta Odontol Scand. 2006;64:104-10.
Bufersen S, Jones J, Shanmugham J, Hsu TY, Rich S, Ziyab AH, Chogle S. Survival of endodontically treated permanent teeth among children: a retrospective cohort study. BMC Oral Health. 2021;21:589.
Arya S, Duhan J, Tewari S, Sangwan P, Ghalaut V, Aggarwal S. Healing of apical periodontitis after nonsurgical treatment in patients with type 2 diabetes. J Endod. 2017;43:1623-7.
Sebring D, Jonasson P, Buhlin K, Lund H, Kvist T. Endodontiska infektioner och allmänhälsa. Tandläkartidningen. 2020;2:64-71. (Also published the other Nordic Dental Journals).
Meurman JH, Janket SJ, Surakka M, Jackson EA, Ackerson LK, Fakhri HR, Chogle S, Walls A. Lower risk for cardiovascular mortality for patients with root filled teeth in a Finnish population. Int Endod J. 2017;50:1158-1168.
Liljestrand JM, Salminen A, Lahdentausta L, Paju S, Mäntylä P, Buhlin K, Tjäderhane L, Sinisalo J, Pussinen PJ. Association between dental factors and mortality. Int Endod J. 2021;54:672-681.
Mannocci F, Bhuva B, Roig M, Zarow M, Bitter K. European Society of Endodontology position statement: The restoration of root filled teeth. Int Endod J. 2021;54:1974-81.
Naumann M, Schmitter M, Frankenberger R, Krastl G. „Ferrule comes first. Post is second!” Fake news and alternative facts? A systematic review. J Endod. 2018;44:212-9.
Dawood A, Patel S. The Dental Practicality Index - assessing the restorability of teeth. Br Dent J. 2017;222:755-8.
Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J. 2009;42:757-74.
Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod. 2008;34:1302-5.
Pennington MW, Vernazza CR, Shackley P, Armstrong NT, Whitworth JM, Steele JG. Evaluation of the cost-effectiveness of root canal treatment using conventional approaches versus replacement with an implant. Int Endod J. 2009;42:874-83.
Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature -- Part 2. Influence of clinical factors. Int Endod J. 2008;41:6-31.
Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod. 2012; 38: 1170-6.
Yu VSH, Messer, HH, Yee R, Shen L. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endod. 2012;38:41-6.
Strindberg LZ. The dependence of the results of pulp therapy on certain factors. Acta Odontologica Scandinavica 1956;14:Suppl 21.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006; 39,:921–930.
Kvist T. Endodontic retreatment. Aspects of decision making and clinical outcome. Swed Dent J Suppl. 2001;144:1-57.
Reit C, Kvist T. Endodontic retreatment behavior: the influence of disease concepts and personal values. Int Endod J. 1998;31:358-63.
Kvist T, ed. Apical periodontitis in root-filled teeth: endodontic retreatment and alternative approaches. 2018: Cham: Springer International Publishing.
Corresponding author: Thomas Kvist. E-mail-address: kvist@odontologi.gu.se
Accepted for publication .06.08.2022
The article is peer reviewed.
Kvist T. Hofmann B, Brodén J, Tjäderhane L. Uncertainties and decision making in endodontics. Nor Tannlegeforen Tid. 2023; 133: 114-20.
Key words: endodontology, decision-making, uncertainty
Artikkelen er fagfellevurdert.
Artikkelen siteres som:
Kvist T, Hofmann B, Brodén J, Tjäderhane L. Uncertainties and decision making in endodontics. Nor Tannlegeforen Tid. 2023;133:114-20. doi:10.56373/2023-2-7
