Oral health of children and adolescents – factors of concern in the future
Abstract
Oral health of children and adolescents – factors of concern in the future
In children, oral health is an integral part of general health. Good oral health contributes to normal growth and development as well as good quality of life. Professionals working with children should be aware not only of normal growth and development, but also of the special needs of children and how to take into account all the information concerning them in dental care. Good oral health is not a given for healthy children, let alone those suffering from illness.
Caries continues to be a problem, and early childhood caries (ECC) can lead to severe oral infections and even repeated treatment requiring general anaesthesia. Today, caries is still predictive of caries. Signs of risk of periodontitis can be seen as early as during the deciduous teeth phase. Both illnesses have long-term impacts; on the other hand, both can be managed with good early diagnostics and by intervening when the disease is still preventable.
As many as one in every five children has a chronic systemic illness, the most prevalent being allergies, asthma, diabetes and autoimmune diseases, of which rheumatoid arthritis is the most common. Nearly 10 % of children suffer from mental problems. Changes in the way people eat, a more sedentary lifestyle and increased screen time have led to a rise in the prevalence of obesity among children and adolescents. While smoking has become less prevalent the use of snuff has become more common among adolescents. All this poses a threat to oral and general health in the future.
Dental practitioners must be prepared to assess whether a child’s right to a safe environment, normal growth and development and good health is met. Promotion of oral health must be continuous on population as well as on individual level, and new methods to achieve this need to be developed. All children have the right to good oral health.
Headlines
Continuous oral health promotion is essential at population as well as individual level – caries and periodontal disease persist among children.
Systemic and psychiatric diseases, as well as neuro developmental disorders are common among children, affect oral health, and therefore must be born in mind in dental treatment planning.
Overweight is today’s problem and threatens both child’s general and oral health, the same is true for eating disorders, although rare.
Problems in maintaining child’s oral health concerns the entire family.
Dental professionals possess a key role in detecting child’s health being neglected by care takers.
Introduction
The child’s development and growth is a bio-psycho-social cascade where the development in all three era is necessary and problems in any of them interfere with normal growth. Parents, dental and medical professionals as well as the society are responsible for guaranteeing a healthy environment, child’s undisturbed development, and health. According to The United Nations Convention on the Rights of the Child article 24 (1) every child has the right to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and rehabilitation of health. Along with the right to evaluation and support of somatic development and health, every child and family has similar right for psychosocial development and welfare (2). Good oral health is an essential part of general health and necessary for growth and development. On the other hand, poor oral health is a risk for general health and systemic diseases may be a threat to oral health. (figure 1)

Figure 1. Good oral health is essential for health and wellbeing of all children. The photo was taken in the Oulu University Hospital Finland for this purpose with the written consent of the mother.
Systemic and psychiatric diseases and weight
Systemic diseases
Even one fifth of Finnish children have a chronic systemic disease with varying severity. The most common are allergies, asthma, neurodevelopmental disorders, coeliac disease, type I diabetes (DM I) and autoimmune diseases of which juvenile idiopathic arthritis (JIA) is the most common. The proportion of children diagnosed with obesity, inflammatory bowel disease (IBD), DM I, and JIA as well as with organ transplants, operated heart conditions and the survivors of childhood cancer, has been increasing in recent years (3). In Finland, 500 children (<1 %) and adolescents are diagnosed with DM I annually, while the number is 400 children for congenital heart diseases and 150 children for JIA. Chronically ill children often have a higher risk of oral diseases compared with their healthy peers and they have special needs in dental care. For example, children with congenital heart disease comprise a risk group for dental caries (4) and diabetics are prone to gingivitis and have greater plaque accumulation (5). JIA often involves the temporomandibular joint and thereby affects the developing occlusion (6). If left untreated, poor oral health can have a devastating impact on the overall health, especially for those with certain systemic health problems and conditions. Lack of preventive and timely therapeutic care may exacerbate systemic problems. Oral health care of patients with systemic health problems often necessitates consultation with the medical specialists who treat the child and treatment may need to be rendered in hospital settings. Having pathways to ensure children’s oral health at appropriate level and way needs continuous attention
High and low BMI
In recent years snacking has replaced regular meals. Consumption of soft and energy drinks has increased, causing a threat for general as well as oral health (7). Frequent snacking and intake of sweet products are associated with overweight (8), but also with dental caries (9). Indeed, children’s overweight and obesity are common in today’s industrialized world (10). Simultaneously with dietary changes, time spent in front of TVs, PCs and mobile applications has increased at the expense of physical activity, in particular among the teens (11). Literature of the association between overweight and caries is contradictory; both high and low BMI have been shown to associate with decaying. The association appears different in countries of different developing stage (12). These issues need close monitoring in future.
Eating disorders, on the other hand, are common especially among girls, when approximately 7 % of Finnish women get such diagnosis before 30 years of age (13). Eating disorders threaten general as well as oral health. The most remarkable problem is dental erosion, in which teeth dissolve due to frequent vomiting or consumption of acid food and drinks (14) combined with occlusal forces. The prevalence of erosive tooth wear per se is increasing and a matter of concern especially among the young.
In all cases where a young patient has an eating disorder of any kind, possibility for professional nutritional counselling must be considered, in some cases even counselling to arrest erosive tooth wear. It is important to remember that an eating disorder may be a symptom of an underlying mental problem, which requires referral to psychiatric counselling.
Visions in child psychiatry
In a Finnish population-based study (n=2682) by Borg and coworkers (15), 17 % of children aged 4–9 years were reported to have psychiatric symptoms according to the Strength and Difficulties Questionnaire (SDQ, www.sdqinfo.com) filled in by parents and / or teachers. Based on the reports by physicians working in primary health care clinics, 12 % of children and families were evaluated to need treatment and support in primary health care and respectively 9 % (number of reports 2604) in specialized health care due to psychosocial problems.
There is no evidence of substantial increase in children´s mental health problems in Finland between 1989 and 2013; however, the use of mental health services has constantly increased (16). The number of referrals indicates better detection of children´s mental health problems but it might also indicate that children with mental health problems have substantial difficulties to cope in a more complex operational and emotional daily environment. Recognition of risk factors, early detection as well as prevention and care of psychosocial problems is both effective and cost-efficient (2).
Psychosocial aspects should be taken into account in every contact with a child in health care system, including dental care. All health care personnel are responsible to detect the possible risk factors and / or psychiatric symptoms and organize or refer the child and the family to appropriate evaluation, care and support. The common goal is to provide good mental health.
Children and adolescents with psychiatric issues may have difficulty even in attending routine dental check-ups and with coping with dental treatment. Again, medications may cause a reduced salivation rate and a child’s/adolescent’s motivation for good homecare maybe low, which all increase risk i.e. for dental caries. Therefore, preventive measures should be carried out frequently by the professionals and these children/adolescents should have shortened recall intervals. If necessary, for instance due to large treatment need or symptoms, these children should be treated under dental general anesthesia (DGA).
Neurodevelopmental disorders
Neurodevelopmental disorders affect about 10 % of the general child population, and the most common types being attention deficit hyperactivity disorder (ADHD) occurring in 3–6 %, language impairment in 5 %, intellectual disability in 1–2 %, autism spectrum disorders (ASD) in 1.5 %, and Tourette Syndrome and Obsessive Compulsive Disorder (OCD) in 1 %. Comorbidity between neurodevelopmental disorders is common, i.e. 50 % of children with ASD also fulfil diagnostic criteria for ADHD. Because most neurodevelopmental disorders present symptoms already at an early age, long before reaching a certain diagnosis, a concept of ESSENCE (Early Symptoms of/Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations) has been presented to be used for this group (17), implementation of which is a future challenge.
Dental behavior management problems are common in children with neurodevelopmental disorders (18). Such children gain from a structured dental appointment (e.g. 1000-learning), and especially children with ASD from augmentative communication (e.g. using pictures). In ADHD, executive dysfunctions lead to difficulties using previous dental experiences to decide how to react during the present dental appointment (19). ASD is characterized by impairments in social interaction and communication, restricted patterns of behavior, and unusual sensory sensitivities (DSM-5 2013). Children with ASD are impaired in building flexible predictions and expectations, which is very much needed during a dental visit. Sensory abnormalities to a greater extent affect those with severe autistic traits (20). However, in the dental setting, bright light, loud noises and strong tastes or smells offer a challenge even for those with milder sensory sensitivities.
Variable |
Group n ( %) |
p |
||
|---|---|---|---|---|
DGA |
Control |
|||
Fearful parent |
22 (25.3) |
8 (7.8) |
0.001 |
|
DGA of parent |
10 (11.5) |
8 (7.8) |
n.s. |
|
DGA of sibling |
15 (17.2) |
4 (3.9) |
0.009 |
|
Number of children in the family |
1 |
6 (6.9) |
16 (15.5) |
0.039 |
2 |
26 (29.9) |
39 (37.9) |
||
3 |
22 (25.3) |
28 (27.2) |
||
≥4 |
30 (34.5) |
19 (18.4) |
||
Oral health
Dental caries
Caries still is the most common chronic disease worldwide (21). If left untreated, dental caries can cause toothache, loss of function, and even dental infections that may even become life threatening. Caries with its consequences may deteriorate child’s oral health related quality of life (OHRQoL) (22) affecting child’s sleeping, playing, eating and self-esteem (23). ECC, early childhood caries, concerns only a minority of children, but deteriorates life of the children and people around them. It is often a reason for referral to DGA, even more than once (24) (figure 2).

Figure 2. ECC – Early Childhood Caries is the most common reason for dental general anesthesia (DGA) among children. Due to anatomical characteristics, progress of dental caries in primary teeth is faster than in permanent teeth.
Literature on DGAs has revealed background factors related to both family issues and negative oral health behaviors (25) (Table 1). Removing plaque and using fluoride toothpaste twice per day (26) and favoring healthy diet without snacking (27) are the means for controlling and preventing manifestations of caries disease. Oral health must not be taken for granted, but promotion must be continuous at population level. When treating children with risk for caries, it is most important to get families involved and aim to support them and help child with individual plan for caries controlling. It must always be borne in mind that DGA is not without risks. Indeed, research is needed to identify the potential risks associated with the use of general anesthesia especially for the very young children.
Periodontal disease
Children and young individuals also suffer from periodontal diseases. Plaque accumulation at the gingival margin is the major cause of gingival inflammation, which results in an environment favoring inflammophilic bacteria and may lead to a dysregulated immune response and, further, to the initiation of periodontal destruction (28). Gingivitis is common among the toddlers, but also signs of periodontitis (i.e. loss of marginal bone) can be detected already in the primary dentition. A study using bitewing radiographs, bone loss for at least one proximal site was prevalent in 4.5 % of 9-year-olds (29). In a longitudinal study the presence of subgingival calculus was connected to progression of periodontitis on periodontal conditions among teenagers (30). Smoking as well as diabetes are known to expose to periodontal disease. Association of diabetes with gingival inflammation and attachment loss was shown in a cohort study with 700 children and adolescents, and periodontal destruction was shown to occur even under the age of 12 years (31). Some evidence exists also on the association between the extent of gingival bleeding and metabolic syndrome in 8‐ to 10‐year‐old children, specifically boys (32). It is notable that in addition to local tissue damage, chronic infection in the periodontium may lead to low-grade systemic inflammation, which is associated with several systemic diseases. Careful diagnostics and considering the risk factors, are essential for detection of the disease at its early phase, and early intervention is of utmost importance in preventing the development of advanced periodontal disease and likely in providing support for general health. If any signs of aggressive periodontal disease are seen in a child, the child should be referred to a specialist in periodontology, or he/she should be consulted.
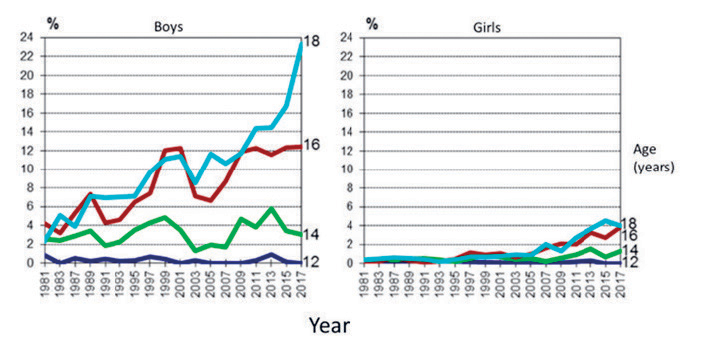
Figure 3. Proportion of 12 to 18 -year-olds, who use snuff (snus) occasionally or daily in 1981–2017 (Adolescent Health and Lifestyle Survey 2017). Kinnunen J, Pere L, Raisamo S, Katainen A, Ollila H, Rimpelä A. The Adolescent Health and Lifestyle Survey 2017: Adolescent smoking, alcohol use and gambling. Reports and Memorandums of the Ministry of Social Affairs and Health 2017:28.
Threat of future consequences of childhood oral infections
A recent article by Pussinen et al. (2019) (33) showed that oral infections in childhood, such as the signs of either periodontal disease or dental caries or both was associated with the subclinical carotid atherosclerosis in early 30’s despite other risk factors for cardio vascular disease. The risk appeared to be even higher for boys. This was a path finder study in this era, and the findings emphasize the importance of a child’s oral health.
Neglecting the child
Neglecting a child’s oral health and home care may be the only signs of child maltreatment. However, this is clinically obvious for any dentist. The most vulnerable group for maltreatment is small children. The prevalence of untreated dental caries has been found to be increased among maltreated, sexually and physically abused children (34). Signs like abnormal bruises in oro-facial region may raise suspicion for child´s sexual or physical abuse. Maltreatment can have lifelong effects on child´s mental and physical development (35). Evaluation of child´s sexual or physical abuse is demanding and needs multidisciplinary approach. In Finland, there are teams, including a dentist in every university hospital specialized in evaluating child abuse cases. If a concern arises about child maltreatment, a dentist is obliged to inform the local authorities responsible for children’s protection.
Smoking and snuff use
Literature shows decline in smoking prevalence among adolescents, whereas snuff or «snus» use is common in all Nordic countries including Finland (36–38) (figure 3), where selling snuff is not legal. Snuff is traditionally used by athletes active in team sports (39), but with increasing trend, the use is increasing among all teens. Snuff can cause strong addiction due to its´ nicotine content. Health effects of snuff use depend on the dose as well as length of snuff use. Smoking adolescents seem to be prone to an outbreak and progress of periodontitis compared to non-smokers (40). It has been shown that an immediate effect of a snuff dose is increase in heart rate and blood pressure (41) Long-term snuff use has been shown to be associated with general health such as cardiovascular diseases (42), diabetes type 2 (43), as well as being potentially carcinogenic (44). In addition, «snus» use has been found to be associated with increased risk of premature birth, stillbirth, and lower birth weight (45). In vivo and in vitro studies about health effects of snuff use are needed to understand the role of snuff in diseases. Even questioning about the use of tobacco products has shown to be effective, therefore dentists should make a routine of asking even their young patients on the use of tobacco products and motivate and support them to stop the possible use.
Conclusion
While treating a child, a dentist must be aware of the child’s physical and mental developmental state, as well as any systemic diseases or neurologic or psychic disturbances. He/she should also be able to treat the child according to the developmental stage and considering any special needs. The dentist should be able to follow the child through the early years in collaboration with the whole team of dental professionals closely communicating with the family to support their commitment. It is essential that the dentist knows when and where to refer the child if needed. There must be a sufficient number of pediatric dentists for referring and consulting. Also, pathways must exist to ensure the collaboration between pediatric dentists and those working in primary health care. Information on the latest methods for prevention and treatments in pediatric dentistry must be delivered to all those involved in taking care of the child whether at home, day care, dental offices or hospitals.
Every child, including those with special needs are entitled to individual treatment plan, health promotion, and continuous monitoring. Population-based oral health promotion should be continuous adopting new ways for it. Oral health cannot be taken for granted. There is global alliance with an aim that children born in 2025 and after that will no more have manifested caries lesions. For now, the success in reaching that goal is controlling the causes known to be associated with oral diseases, mainly microbes, and diet, and for dental caries using regularly topical fluoride products. Maybe the ongoing research on the role of microbiota and genetics will bring new insight for controlling oral diseases. The aim of all health personnel must be to ensure the best possible oral health for children.
References
United Nations Convention on the Rights of the Child. (1989). https: //downloads.unicef.org.uk/wp-content/uploads/2010/05/UNCRC_united_nations_convention_on_the_rights_of_the_child.pdf?_ga=2.243028614.587544160.1553328086–1029161349.1553328086 Entered 26.3.2019
Kilian R, Losert C, Park A-La , McDaid D, Knapp M. Cost-Effectiveness Analysis in Child and Adolescent Mental Health Problems: An Updated Review of Literature. International Journal of Mental Health Promotion. 2010; 12: 45–57.
Tapanainen P, Rajantie J. Chronic diseases. in Rajantie J, Heikinheimo M, Renko M, eds. Pediatrics, 6th edition. Helsinki: Duodecim 2016; 74–8.
Stecksén-Blicks C, Rydberg A, Nyman L, Asplund S, Svanberg C. Dental caries experience in children with congenital heart disease: a case control study. Int J Paediatr Dent 2004; 14: 96–100.
Ismail AF, McGrath CP, Yiu CK. Oral health of children with type 1 diabetes mellitus: A systematic review. Diabetes Res Clin Pract. 2015; 108: 369–81.
Hsieh YJ, Darvann TA, Hermann NV, Larsen P, Liao YF, Bjoern-Joergensen J, Kreiborg S. Facial morphology in children and adolescents with juvenile idiopathic arthritis and moderate to severe temporomandibular joint involvement. Am J Orthod Dentofacial Orthop. 2016; 2: 182–91.
Visram S, Cheetham M, Riby DM, Crossley SJ, Lake AA. Consumption of energy drinks by children and young people: a rapid review examining evidence of physical effects and consumer attitudes. BMJ Open. 2016; 6: e010380.
Kumar S, Kroon J, Lalloo R, Kulkarni S, Johnson NW. Relationship between body mass index and dental caries in children, and the influence of socio-economic status. Int Dent J. 2017; 67(2): 91–7.
Evans E W, Hayes C, Palmer CA, Bermudez OI, Cohen SA, Must A. Dietary intake and severe early childhood caries in low-income, young children. J Acad Nutr Diet. 2013; 113: 1057–61.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006; 1: 11–25
Pate RR, Mitchell JA, Byun W, Dowda M. Sedentary behaviour in youth. Br J Sports Med. 2011; 45: 906–13.
Hooley M, Skouteris H, Boganin C, Satur J, Kilpatrick N. Body mass index and dental caries in children and adolescents: a systematic review of literature published 2004 to 2011. Syst Rev. 2012; 21; 1–26.
Keski-Rahkonen A, Hoek HW, Linna MS, Raevuori A, Sihvola E, Bulik C et al. Incidence and outcomes of bulimia nervosa: a nationwide population based study. Psychol Med. 2009; 39: 823–31.
Lo Russo L, Campisi G, Di Fede O, Di Liberto C, Panzarella V, Lo Muzio L. Oral manifestations of eating disorders: a critical review. Oral Dis. 2008; 14: 479–4.
Borg, A-M. Early detection of children’s mental health problems. Dissertation. Acta Universitatis Tamperensis 2076, Tampere University Press, Tampere, Finland. 2015. https: //tampub.uta.fi/bitstream/handle/10024/97896/978–951–44–9864–0.pdf?sequence=1
Sourander A, Lempinen L, Brunstein Klomek A. Changes in mental health, bullying behavior and service use among 8-year-old children during 24 years. J Am Acad Child Adolesc Psychiatry. 2016; 55: 717–25.
Gillberg C. The ESSENCE in child psychiatry: Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations. Res Dev Disabil 2010; 31: 1543–51.
Stein L, Lane C, Williams M, Dawson E, Polido J, Cermak S. Physiological and behavioral stress and anxiety in children with autism spectrum disorders during routine oral care. Biomed Res Int. 2014; 2014: 694876.
Blomqvist M, Holmberg K, Fernell E, Ek U, Dahllöf G. Dental caries and oral health behavior in children with attention deficit hyperactivity disorder. Eur J Oral Sci 2007; 115: 186–91.
Klintwall L, Holm A, Eriksson M, Carlsson LH, Olsson MB, Hedvall A, Gillberg C, Fernell E. Sensory abnormalities in autism – a brief report. Res Dev Disabil. 2011; 32: 795–800.
Kassebaum NJ, Smith AGC, Bernabe E. Fleming TD, Reynolds AE, Vos T et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res 2017; 96: 380–7.
Meyer F, Enax J. Early Childhood Caries: Epidemiology, Aetiology, and Prevention. Int J Dent. 2018; 22: 415873.
Acs G, Shulman R, Ng MW, Chussid S. The effect of dental rehabilitation on the body weight of children with early childhood caries. Pediatr Dent.1992; 21: 109–13.
Sheller B, Williams BJ, Hays K, Mancl L. Reasons for repeat dental treatment under general anesthesia for the healthy child. Pediatr Dent. 2003; 25: 546–52.
Rajavaara P, Laitala ML, Vähänikkilä H, Anttonen V. Oral health behaviors associated with dental general anesthesia among healthy children. Adv Pediatr Res. 2018; 5: 3.
Marinho V C, Higgins JP, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003; 4: CD002782.
Marshall TA, Broffitt B, Eichenberger-Gilmore J, Warren JJ, Cunningham MA, Levy SM. The roles of meal, snack, and daily total food and beverage exposures on caries experience in young children. J Public Health Dent. 2005; 65; 166–73.
Sanz M, Beighton D, Curtis MA, Cury JA, Dige I, Dommisch H, Ellwood R, Giacaman RA, Herrera D, Herzberg MC, Könönen E, Marsh PD, Meyle J, Mira A, Molina A, Mombelli A, Quirynen M, Reynolds EC, Shapira L, Zaura E. Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases. Consensus report of group 1 of the Joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J Clin Periodontol 2017; 44 (suppl 18): S5-S11.
Sjödin B, Arnrup K, Matsson L, Wranne L, Carlsson J, Hänström L. Periodontal and systemic findings in children with marginal bone loss in the primary dentition. J Clin Periodontol. 1995; 22: 214–24.
Clerehugh V, Lennon MA, Worthington HV. 5-year results of a longitudinal study of early periodontitis in 14- to 19-year-old adolescents. J Clin Periodontol. 1990; 17: 702–8.
Lalla E, Cheng B, Lal S, Kaplan S, Softness B, Greenberg E et al. Diabetes mellitus promotes periodontal destruction in children. J Clin Periodontol. 2007; 34: 294–8.
Kå K, Rousseau MC, Lambert M, Tremblay A, Tran SD, Henderson M et al. Metabolic syndrome and gingival inflammation in Caucasian children with a family history of obesity. J Clin Periodontol. 2013; 40: 986–93.
Pussinen PJ, Paju S, Koponen J, Viikari JSA, Taittonen L, Laitinen T, Burgner DP, Kähönen M, Hutri-Kähönen N, Raitakari OT, Juonala M. Association of childhood oral infections with cardiovascular risk factors and subclinical atherosclerosis in adulthood. JAMA Netw Open. 2019; 2 : e192523.
Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high- income countries. Lancet. 2009; 373: 68–81.
Valencia-Rojas N, Lawrence HP, Goodman D. Prevalence of early childhood caries in population of children with history of maltreatment. J Public Health Dent. 2008; 68: 94–101.
Statistics Sweden. Tobacco habits by indicator, age and sex. Percentage and estimated numbers in thousands. Year 2008–2009–2016–2016- Latest update 4/2017. Available from; http: //www.statistikdatabasen.scb.se/pxweb/en/ssd/START__LE__LE0101__LE0101H/LE0101H25/?rxid=4c116499–0bf1–4215–947b-5d046c0a9e10
Statistics Norway. Smoking habits. Latest update 1/2018. Available from: https: //www.ssb.no/en/statbank/table/07692/tableViewLayout1/?rxid=9761759f-b49c-45c5-bcd5-f0ec169e6477
Kinnunen JM, Pere L, Raisamo S, Katainen A, Ollila H, Rimpelä A. The Adolescent Health and Lifestyle Survey 2017: Adolescent smoking, alcohol use and gambling Available from: http: //julkaisut.valtioneuvosto.fi/bitstream/handle/10024/80160/V2_kirjanmerkit_20170824_Suomi %20100_NTTT2017_korjaukset_mukana %20(2).pdf
Mattila VM, Raisamo S, Pihlajamäki H, Mäntysaari M, Rimpelä A. Sports activity and the use of cigarettes and snus among young males in Finland in 1999–2010. BMC Public Health. 2012; 12: 230.
Heikkinen AM, Pajukanta R, Pitkäniemi J, Broms U, Sorsa T, Koskenvuo M, Meurman JH. The effect of smoking on periodontal health of 15- to 16-year-old adolescents. J Periodontol. 2008; 79: 2042–7.
Martin JS, Beck DT, Gurovich AN, Braith RW. The acute effects of smokeless tobacco on central aortic blood pressure and wave reflection characteristics. Exp Biol Med. 2010; 235: 1263–8.
Foulds J, Ramstrom L, Burke M, Fagerström K. Effect of smokeless tobacco (snus) on smoking and public health in Sweden. Tob Control. 2003; 12: 349–59.
Carlsson S, Andersson T, Araghi M, Galanti R, Lager A, Lundberg M et al. Smokeless tobacco (snus) is associated with an increased risk of type 2 diabetes: results from five pooled cohorts. J Intern Med. 2017; 281: 398–406.
IARC, IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol. 89, Smokeless Tobacco and Some Tobacco-specific N-Nitrosamines. International Agency for Research on Cancer, Lyon, France, 2007. Available from: https: //www.iarc.fr/en/publications/pdfs-online/prev/handbook14/handbook14.pdf
Baba S, Wikström AK, Stephansson O, Cnattingius S. Influence of snuff and smoking habits in early pregnancy on risks for stillbirth and early neonatal mortality. Nicotine Tob Res. 2014; 16: 78–83.
Corresponding author: Vuokko Anttonen, POB 5281, 90014 University of Oulu, Finland. E-mail: vuokko.anttonen@oulu.fi
Accepted for publication 10 June 2019.
This paper has been peer reviewed.
Anttonen V, Blomqvist M, Alapulli H, Methuen M, Koskinen S, Yli-Urpo H, Rajavaara P, Tanner T, Lindholm P, Könönen E. Oral health of children and adolescents – factors of concern in the future. Nor Tannlegeforen Tid. 2020; 130: 18–24
MeSH: Children; Dental Caries; Periodontal Diseases; Health; Body Mass Index; Tobacco, Smokeless; Anaesthesia, General
Artikkelen er fagfellevurdert.
Artikkelen siteres som:
Anttonen V, Blomqvist M, Alapulli H, Methuen M, Koskinen S, Yli-Urpo H, Rajavaara P, Tanner T, Lindholm P, Könönen E. Oral health of children and adolescents – factors of concern in the future. Nor Tannlegeforen Tid. 2020;131:18-24. doi:10.56373/2020-1-5