Assessment of patients with severe temporomandibular disorder in Norway - a multidisciplinary approach
Norway is in the process of establishing a national program for patients with refractory orofacial pain (TMD). The program comprises a systematic multidisciplinary evaluation with a two year follow-up, together with national evidence-based guidelines on the evaluation and treatment of TMD. This paper describes the establishment of the evaluation program and current results.
Temporomandibular disorder (TMD) is a disabling state for many patients. The symptoms are moderate to severe pain in the orofacial area, including the masticatory muscles, and/or the joint (temporomandibular joint derangement, TMJD). In addition, there may be associated comorbidity such as ear pain, tinnitus, dizziness, neck pain, tension- and migraine headache, chronic fatigue, fibromyalgia, depression, allergies and irritable bowel syndrome (1). Although the symptoms may often be mild and self-limiting, some patients can experience acute onset of severe symptoms and the condition may develop into a persistent pain problem with physical, behavioral, psychological and psychosocial symptoms (2). Recent findings in the Prospective Evaluation and Risk Assessment (OPPERA) case-control study have demonstrated that patients with TMD may differ from healthy persons with regard to sociodemographic factors, clinical variables, psychological function, pain sensitivity and autonomic domains (3). Lifestyle factors such as diet may have implications for chronic pain, including TMD (4, 5).
As early as the late nineties a number of reports from the dental field advocated multidisciplinary management of TMD patients with focus on psychological factors (6 - 8). Psychological stress has been highlighted as a factor that can contribute to the sensation of pain and the development of TMD (9). Velly et al. found that depression and catastrophizing are factors that can contribute to the progression of pain and disability in patients with chronic temporomandibular muscles and joint diseases (10). Ahmed et al. in the UK recently described a multidisciplinary TMD team involving both dental and medical specialists (11). In this model patients are referred from primary, secondary and tertiary care when routine treatments have failed. They are triaged by a maxillofacial surgeon and on discharge they return to the referring general practitioner for care. The authors found improvement in pain intensity scores and mandibular function, as well as improved quality of life outcome measures. Zakrzewska gives an overview of additional factors, emphasizing the complex etiology of orofacial pain and the need for accurate diagnosis and a biopsychosocial approach (12). The facial area is «shared» by dental and medical professions. This may cause confusion, especially when there is no communication between the involved specialists.
Temporomandibular disorders (TMD) in Norway
The TMD patient society («TMD foreningen») recently made a strong case to the Norwegian health authorities. TMD society patients had typically undergone numerous investigations and interventions, without success. Some of them had sought healthcare abroad at private clinics in the UK, Germany and the USA. These treatments were expensive (NOK 200,000 - 600,000), lacked scientific documentation, had limited effect and had to be funded by the patients themselves. The TMD society felt that the Norwegian health care system did not take the patient group seriously and that it was unable to provide adequate diagnostic work-up and treatment. The society was consistently active in lobbying politicians who in turn raised questions in parliament to the Minister of Health and Care Services(13). As a result the Norwegian Directorate of Health was given a mandate from the Ministry of Health and Care Services to initiate a program designed to help this particular group of patients.
The Department of Oral and Maxillofacial Surgery at Haukeland University Hospital in Bergen agreed to design a multidisciplinary program for this patient group. After consulting a number of medical and dental specialties, including orthopedics, neurology, ENT, and psychosomatic medicine, a working collaboration was formed between the Departments of Oral and Maxillofacial Surgery, Prosthodontics, Orthodontics and the Pain Clinic (Centre for Pain Management and Palliative Care) at Haukeland University Hospital, Bergen. The pain clinic has 30 years' experience providing multidisciplinary evaluation of chronic pain and has an integrated model with 3 clinical teams; an outpatient clinic for chronic noncancer pain, an acute pain team and a palliative care team (14). Maxillofacial imaging was included in the project to ensure Magnetic Resonance Imaging (MRI) diagnostics of the temporomandibular joint. Haukeland University Hospital is the regional hospital for Western Norway serving a population of almost 1.1 million. During the development of the multidisciplinary program collaboration was also initiated with the Oral and Maxillofacial Pain Center at the Massachusetts General Hospital in Boston, USA (15).
Another focus area was the need for national guidelines. In 2013 a working group at the Norwegian Health Ministry was established for the development of national guidelines for good clinical practice for the diagnosis and treatment of individuals with TMD (16). Two of the authors of this paper work in the guideline group. The TMD guidelines are intended to provide clinically practical recommendations on diagnosis, treatment, referrals, monitoring and interdisciplinary cooperation. Literature searches have been performed including the Swedish Council on Medical Assessment (SBU) (17); Socialstyrelsens guidelines for Oral physiology- pain and functional disorders of the mouth, face and jaw (18); the Finnish and Japanese reports of guidelines for orofacial pain and TMD and the UpToDate report (19).
The aim of this report is to describe the Norwegian national multidisciplinary program for patients with refractory orofacial pain (TMD). Multidisciplinary in this context means collaboration between dental specialists and pain clinic specialists within the Health care system.
The multidisciplinary evaluation
The program includes patients with severe TMD symptoms referred from all health care regions in Norway. The patients are referred by his/ her primary care physician. Inclusion in the program is based on severity of symptoms, duration of symptoms and consequences such as extended periods of sick-leave and disability pension. Prior to the initial visit the patients complete a comprehensive questionnaire including family- and pain history, jaw function (mandibular function impairment questionnaire, MFIQ (20)), lifestyle factors (sleep, diet, caffeine) and validated measures of anxiety and depression (HADS (21), Roland scale, catastrophizing questions (22)).
The patient is seen on four separate days by dental specialists, radiologists and members of the pain clinic team (Fig. 1). At the final consultation a dynamic feedback meeting takes place to present the results and treatment recommendations (Fig. 2).
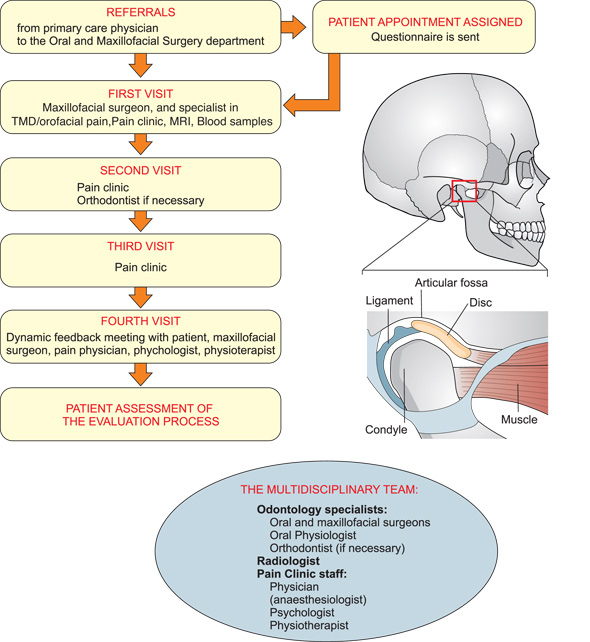
Fig 1: The patient is seen on four separate days by dental specialists, radiologist and members of the pain clinic team.
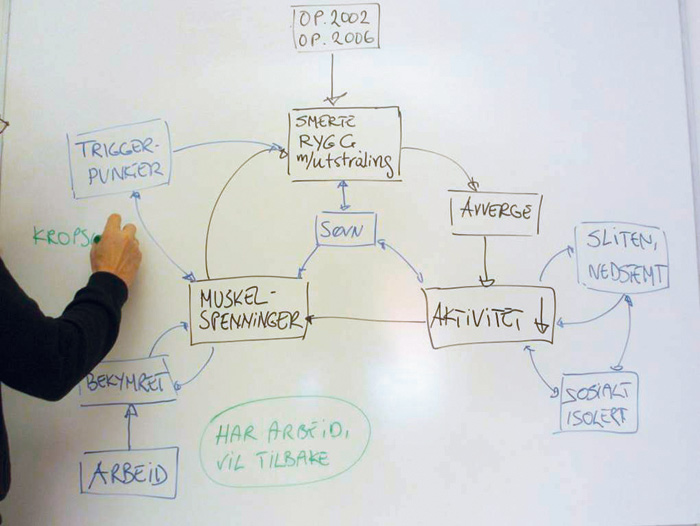
Fig 2: A dynamic feedback meeting. After the multidisciplinary team has presented the team findings to the patient the whiteboard is used to illustrate how the symptoms have developed and the different factors influencing the pain. It is important that the patient comprehends and accepts this explanation which then provides a basis for treatment suggestions. (Illustration by psychologist Borrik Schjödt).
At the initial consultation orthopantograms (OPG), clinical photographs, MRI scan, blood- and saliva tests are taken. An oral and maxillofacial surgeon and a specialist in TMD and orofacial pain perform a clinical examination. The purpose of this first step is to detect any condition in the oral and maxillofacial region which could be causing symptoms such as pain and/or restricted jaw movement. Radiology findings are evaluated as an important step in establishing a correct diagnosis of the joints. Orthodontic consultation is also obtained according to predetermined criteria. The patient is subsequently evaluated by a pain physician (anesthesiologist), a clinical psychologist and a physiotherapist at the outpatient clinic at the Centre for Pain Management and Palliative Care. This evaluation involves three separate consultations with an interval of 2 - 3 weeks between each consultation. The time interval is considered advantageous with regard to a cognitive therapeutic perspective. At the final meeting the members of the pain clinic team and the oral and maxillofacial surgeon, have a meeting with the patient, to present and discuss the results of the investigation and a plan for treatment. Following the evaluation, the referring primary care physician receives a detailed report and recommendations for further treatment and care. The primary care physician is responsible for providing any medical treatment recommended by the TMD team, and/or referral to other forms of treatment. If dental treatment is indicated it will be performed by the patient's dentist or if possible, a local specialist in prosthodontics with subspeciality in TMD/orofacial pain. If surgery is necessary, treatment can be given at the Oral and Maxillofacial unit at Haukeland University Hospital. In general it is preferable that the patient receives treatment close to their place of residence.
Clinical examination
All patients undergo a comprehensive examination focused on TMD/TMJ/orofacial pain, comprising a structured interview related to present and past orofacial pain complaints as well as general health, medical history and life style factors.
Dental specialists
The examination carried out by the specialist in TMD/orofacial pain includes palpation of the joints, masticatory and surrounding muscles and an assessment of TMJ function (e.g. deviations, TMJ locking and sounds). The functional and occlusal evaluations include measurement of mandibular movements (maximum opening and horizontal movements) and an assessment of static and dynamic occlusion (e.g. occlusal stability, presence of occlusal interferences, Angle classification, number of occluding contacts). Signs of parafunctional activity are recorded as well (e.g. tongue indentations, cheek biting, attrition facets/tooth wear). The clinical examination followed a routine protocol for assessment of TMD and orofacial pain. Internationally, a diagnostic criterion for TMD (DC/TMD) is often used (23). The protocol is time consuming and with so many dental and medical specialists involved with many overlapping examinations we chose to use a shorter standard examination.
The examination carried out by the Oral and maxillofacial surgeon is focus on the jaw function. Tenderness to palpation over the joint indicates inflammation. If the range of movement on jaw opening is decreased or asymmetry is present it will elicit painful clicking (PC) of the disc or a chronic closed lock (CCL) of the disc in the joint. The examination follows the surgical diagnostic criteria for TMJ (24, 25). The radiographic (OPG) examination includes diagnostics of pathology in teeth and surrounding tissues as a cause of pain. There is also a focus on the joints to exclude anomalies, asymmetries or signs of arthritis.
Facial sensitivity to light touch and pin-prick is examined, and sensitivity and pain thresholds are measured for electrical or pressure stimuli with different devices (pulp vitality tester, Painmatcher and Algometer) (26). Recently we have shown that TMJD patients with limited function of the jaw and movement evoked pain have lower pressure pain thresholds in the orofacial area compared with healthy controls (27). Pain intensity is scored on a numeric rating scale (NRS, 0 - 10; 0= no pain and 10=worst unbearable pain). Salivary cortisol (Salivette cortisol code blue, Sarstedt®) is collected for later mass-spectrometry analyses. An association between pain catastrophizing and elevated salivary cortisol response to experimental pain in TMD patients has recently been demonstrated (28).
Radiologist
MRI is a non-invasive method of examining the TMJ without causing discomfort or harm to the patient. MRI also describes the joint in a way that no previous method has done. The disc and its status are envisaged, and it is possible to see fluid and even minor degenerative changes in both bone and soft tissue, permitting a fairly good impression of possible inflammatory changes. The MRI is performed using a coil specially designed for the area of the TMJ, and with the following sequences: T2W, T1W, STIR and T2W GRE for opening of the mouth. Anterior displacement is described according to a clockwise placement (29). Osteoarthritis is described as severe (3), moderate (2), mild (1) or none (0) (30, 31).
Pain physician (anesthesiologist)
The primary role of the physician in the multidisciplinary pain clinic team is to assess the patient's pain problem from a medical perspective, in relation to prior and current medical history, to determine whether appropriate medical tests have been performed, to rule out underlying illness and to assess whether specific medical treatment is indicated. The assessment includes focus on the efficacy/ tolerability of prior and present drug treatment, the beliefs the patient may have about the etiology of the pain, and current status regarding lifestyle factors (sleep, diet/dietary habits, sedentary lifestyle, use of tobacco, alcohol and/ or stimulants). Appropriate blood tests are conducted. The clinical examination includes the presence or absence of localized or widespread muscular pain, trigger points and/or tender points, likelihood of neuropathic pain, and simple neurological investigation (cranial nerve function, sensory findings, and deep tendon reflexes). Giving the patient an explanation of the pain is of prime importance. Advice to the general practitioner concerning medical treatment includes tapering/cessation of inappropriate or ineffective drugs, and suggestions for alternative drugs if deemed necessary. In addition, where appropriate, advice on sleep, diet and the importance of physical activity, despite the pain.
Pain Clinic psychologist
Psychosocial factors influence the onset, development and continuation of a pain problem. Pain problems influence psychological and social conditions. This applies to chronic pain in general, as well as TMD-related/orofacial pain (Fig. 3).
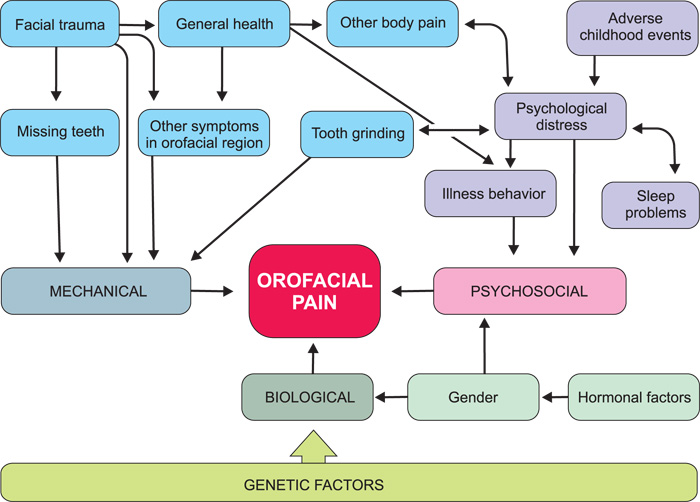
Fig 3: The multifactorial etiology of orofacial pain. From Epidemiology of Orofacial Pain, Macfarlane TV, in Sessle BJ (ed.) Orofacial Pain, IASP Press, 2014.
The role of the psychologist in the team is to assess psychosocial factors relevant for the onset, development and continuance of pain-problems, and assist the patient in formulation of the problem in a way that gives rise to action/a treatment plan.
The clinical assessment is based upon the comprehensive questionnaire filled out by the patient. The psychologist carries out a structured interview, which includes exploring the patient's conception of the problem. The way the patient thinks about the pain problem is known to guide his/her actions - which could worsen the actual problem, or relieve it. It is interesting to map fluctuations of symptoms in relation to other factors (stress, weather conditions, social distractions), because this approach provides ideas for treatment interventions. A large proportion of chronic pain patients, including TMD-patients, have a history of sexual abuse, neglect or other significant negative life-events (31, 32). It is delicate but of vital importance to explore these questions.
It is important to assess the probability of the patient returning to work. The longer the patient stays out of work, the less likely it is that he/ she will return to work. Job satisfaction is probably the second most important factor regarding return to work. Some patients may be in conflict with their insurance companies, or struggling to get worker's compensation. Such conflicts draw attention to the sick-role, making change harder to accomplish.
The psychologist also assesses more obvious psychological factors, like depression, anxiety, cognitive style and function, and coping skills. In this program the Hospital Anxiety and Depression Scale (HADs) was used (21) as well as questions regarding catastrophizing from the One- and two-item versions of the Coping Strategies Questionnaire (CSQ) (22).
Pain Clinic physiotherapist
The aim of the physiotherapy examination is to investigate whether the patient has findings that could affect and enhance chronic pain. The posture may be flexed or extended, with or without protracted head position. Restricted respiratory movements can indicate general tension, and be an indication of the patient`s ability or inability to relax. Palpation may reveal different degrees of muscular elasticity, trigger points and/or tender points. The Global Physiotherapy Examination, GPE-52, contains 52 tests. The test has 5 main domains: posture (8 tests), respiration (8 tests), movement including relaxation tests (16 tests), muscle (12 tests), and skin (8 tests). Every test is scored according to a defined scale. The sum score indicates the degree of problems, but also identifies positive resources. The GPE 52 is validated and reliable (33).
Chronic pain is significantly associated with lack of physical activity/sedentary lifestyle. Assessing the patient`s intensity and frequency of physical activity is important. Some patients with chronic pain exhibit fear- avoidance behavior, which may be an important cause of reduced physical activity and should be investigated.
Patients` assessments of the evaluation process
Each patient is asked to complete a questionnaire with seven statements in order to give their assessment of the evaluation process. The form contains a number of statements, and the respondents are asked to indicate degree of agreement on a continuous scale from 1 (completely agree) to 10 (completely disagree).
Results
The questionnaire
So far 42 patients have been evaluated. Preliminary results show that females dominate (37: 5), mean age 46 years. More than 50 % reported sick leave from work during the last 5 years, a mean of 4.6 times and length of sick leave 17.5 months (mean). Fifty percent of the patients indicated trauma as the likely cause of TMD/TMJ, while 19 % reported general joint hypermobility. Ear symptoms were reported by 86 % of the patients. All had long-lasting pain histories (mean 12.8 years). Most of the patients had elevated scores on the mandibular functional index questionnaire (MFIQ, min=0, max=28, cut off >7) mean 12.7.
The clinical examination by dental specialists:
Pain intensity in the TMD/TMJ area was scored by the patient on a NRS scale 0 - 10. Maximal pain intensity was 8.7 (mean, range 5 - 10). Minimum pain intensity was 2.6 (mean, range 0 - 7). Maximal jaw opening was decreased in 57 % of the patients and 48 % had teeth occlusal interferences. Posterior open bite was found in 10 patients as a result of having used a special splint 24 hours a day. Five cases were diagnosed with caries and 11 with apical periodontitis. Palpation of the jaw muscles showed that 83 % of the patients scored 3 (on a scale 0-5) on palpation of the Pterygoid muscle, 48 % on the Masseter muscle and 67 % on the Temporalis muscle´s insertion onto the mandibular coronoid. A summary of findings from the dental specialists can be seen in Table 1. The cortisol samples and measurements of pain thresholds will be analyzed at a later date.
N |
% |
|
|---|---|---|
Maximal interincisal distance < 40 mm) |
24 |
57 |
Deviation of the jaw in motion |
19 |
45 |
Pain at rest |
41 |
98 |
Pain on jaw movement |
31 |
74 |
Palpation tenderness ( 3 on a 0 - 5 scale) |
||
Pterygoid muscle |
35 |
83 |
Masseter muscle |
20 |
48 |
Temporal muscle insertion |
28 |
67 |
Teeth occlusion interferences |
19 |
48 |
Posterior open bite |
10 |
24 |
Pathology in teeth and/or surrounding tissue |
||
Caries |
5 |
12 |
Apical periodontitis |
11 |
26 |
MRI examination:
MRI showed osteoarthritis in 64 %, most of them mild to moderate findings, but 10 % had severe osteoarthritis, with degenerative destructions in the joints and the disc. In 59 % of patients the disc was anteriorly displaced. Other findings were anomalies of the joint, anatomical changes after old injuries (fractures) and inflammatory changes in both bone and soft tissue.
Pain clinic examination:
On referral six patients (14 %) had a diagnosis of fibromyalgia, eight (19 %) had migraine and four (10 %) had chronic fatigue (ME). A third of patients indicated widespread pain and two third had palpable trigger points. One of the Vitamin D deficient patients also had elevated S-PTH. Two patients had elevated P-Homocystein and five had elevated S-Transferrin receptor. One patient had elevated GF1 and was referred to endocrinological assessment.
Three out of four reported sleep disturbance. There was a high proportion of anxiety and depression, with fifty percent of patients having anxiety and/or depression scores above cutoff. Almost all of the patients had elevated catastrophizing scores.
The physiotherapy examination revealed that fifty percent of the patients had a forward head position, high chest breathing and reduced ability to relax.
A summary of findings from the pain clinic examinations is shown in table 2.
N |
% |
||
|---|---|---|---|
Sleep disturbance |
32 |
76 |
|
Vitamin D deficiency |
8 |
19 |
|
Myofacial trigger points |
31 |
74 |
|
Elevated anxiety score |
8 (on a scale 0-2) |
19 |
45 |
Elevated depression score |
8 (on a scale 0-2) |
12 |
29 |
Patients` assessment of the evaluation process
So far 30 patients have evaluated the program. The overall mean showed a score of 2.25 (see Table III). The evaluation consisted of seven statements regarding how the team treated them, whether they had received explanations of the symptoms and whether their expectations of the process had been met (Table 3).
Statement |
mean |
range |
|---|---|---|
I expect the process to find explanations of my symptoms |
2.6 |
1 - 7 |
I was well received by the team |
1.4 |
1 - 4 |
I consider the team members excellent professionals |
2.0 |
1 - 9 |
I was respectfully received by the team |
1.5 |
1 - 5 |
I received good information during the process |
2.5 |
1 - 6 |
I received adequate information during the process |
2.5 |
1 - 9 |
The process met my expectations |
3.3 |
1 - 9 |
1: completely agree, 10 completely disagree
Treatment recommendations
TMD and orofacial pain
In cases of suspected TMD-related orofacial pain complaints, patients were advised on treatment options, depending on the specific TMD diagnosis. This commonly included conservative treatment modalities such as making the patient aware of daytime parafunctions and bad habits, muscle exercise and oral appliance treatment. Full coverage hard acrylic splints and muscle exercises were recommended for the majority of patients.
Oral and maxillofacial surgery
After conservative treatment for a minimum of 6 months a new evaluation of persisting symptoms is made with focus on the joint (34). In case of PC of the disc two types of surgical options are available, condylotomy or discectomy (35). When the diagnosis is CCL of the disc the first choice is arthroscopy with lysis and lavage (36). If the treatment fails discectomy may be an option (37, 38). Arthroscopy minimizes adherences between the superior surface of the disc and the temporal joint component. Discectomy is performed when the disc is displaced without reduction and acts as an obstacle for condylar movements. In case of osteoarthritis a corticosteroid injection can relive the situation for the patient (39, 40). If severe arthritis is present arthroplasty will be an option (41, 42) So far, eight patients have been treated surgically, two had severe arthritis (including one with PC) and six had CCL. Five cases were treated with arthroscopy including lysis and lavage, one with discectomy and two with artroplasty.
Pain clinic
Suggested treatment included increased physical activity and psychomotoric physiotherapy (43) in 21 (50%) patients. Adjusting ongoing drug treatment (tapering, cessation or another drug) was advised for 32 (76 %) patients. Advice on sleep hygiene was given to 15 (36 %) patients and dietary advice was given to 13 (31 %) patients. Supplementary blood tests were recommended for 4 patients. Eight patients needed Vitamin D treatment. One patient was referred to cardiological examination; one was referred to assessment for sleep apnea. Referral to a psychologist or psychiatrist was recommended for 28 (67 %) patients. Most referrals were based on the need for better coping skills and tendency towards catastrophizing. The majority of patients needed help to accept the situation and to prioritize where they should use their energy. Acceptance and prioritizing are two central questions in ACT - acceptance and commitment therapy - which is considered a new «wave» within cognitive therapies (44). Some patients were recommended treatment for depression.
Discussion
Analyses of data from patients participating in this program may provide useful information regarding identification of risk factors for developing painful TMD, enabling primary health care providers' early identification of patients at risk. Cost-effectiveness will be analyzed as well as how well the patients have been followed up in primary care, in both medical and dental services, following the evaluation and recommendations given by the project team.
This program for patients with severe TMD/TMJ conditions is based on close co-operation between dental and pain clinic specialists. To our knowledge such a tight collaboration has not previously been described in the Nordic countries.
The results so far show that the TMD patients need a multidisciplinary approach. Plans have been made for a two year follow-up to check whether the treatment suggestions have been followed up in primary care and to which extent they have been effective. At the completion of the program a comprehensive report is sent to the referring physician in primary care is responsible for coordination and implementation of the care which is responsible non-dental treatment suggestions. This represents a possible weak link, and it will be interesting to see how well the treatment suggestions are followed up by busy general practitioners.
The evaluation of the process by the patients showed that most of them were very satisfied, especially with how well and respectfully they had been received by the team. Some were less satisfied with how the process had lived up to their expectations, for example disagreeing that they need to be examined by a psychologist. This is interesting, considering that almost all patients scored highly on the test for catastrophizing, fifty percent had anxiety and/or depression scores above cutoff and 67 % were evaluated to be in need of referral to psychologist or psychiatrist.
Chronic pain management requires experience and expertise. All members of the multidisciplinary team have long experience in their respective fields. In addition, collaboration has been established with the Orofacial Pain Center at the Massachusetts General Hospital in Boston, USA which has a similar program.
Arthritis does occur in the TMJ and it is important to screen patients with MRI. Severe arthritis was demonstrated in 10 % of our patients and correlated with clinical findings such as tenderness to palpation over the joints and decreased mandibular function. This condition is diagnosed by the dental specialist together with the radiologist and is often treated by oral and maxillofacial surgeons experienced in treating TMJ pathology. The surgeons in Bergen work in a similar manner to the surgeons in Boston and the surgeons at the Karolinska University Hospital in Huddinge, Sweden. Early treatment may prevent a development into a debilitating chronic condition.
Conclusions
Norway is in the process of establishing a national, multidisciplinary evaluation program for patients with TMD. Based on our data so far, the patients in this program characteristically have a long history of pain. Many have impaired mandibular function, in addition to pain. The majority of patients report sleep disturbances and almost all have elevated catastrophizing scores. Factors such as sedentary lifestyle, suboptimal dietary habits and vitamin deficiencies need to be addressed. Inappropriate drug treatment is another confounding factor. Some patients have underlying medical conditions requiring further investigation. Management of complex pain problems such as refractory TMD requires a multidisciplinary approach.
Clinical relevance for the general dental practitioner
As the prevalence of TMD in the general population is estimated to be between 10 and 15 percent, the general dental practitioner (GDP) will encounter TMD patients on a regular basis. A small proportion of these will develop a long-standing debilitating condition which may be difficult to treat. It is therefore important for the GDP to be able to identify these patients, as early intervention could possibly decrease the risk of chronification. It is also important that the GDP addresses ordinary dental pathology before referring to a multidisciplinary team. TMD patients with catastrophizing tendencies and sleep disturbance may be at risk. The national Norwegian guidelines that are in progress will be finished in 2016 and will be useful for the primary medical- and dental care providers. The guidelines will contribute to better quality of diagnosis, treatment and monitoring of TMD patients. The aim is to ensure that TMD patients are evaluated early. Provision will be made for multidisciplinary collaboration when appropriate and there will be clarification of the reference criteria. The guidelines will highlight how different disciplines can contribute their expertise and in that way facilitate good patient care.
Acknowledgements
We greatly acknowledge the contribution from present and former collaborators: nurses and administrators: Torill Torvund, Tanja Riis, Christin Thompson, Wera Geoghegan; orthodontist Marit Midtbø, radiologist Gunhild Aandal, oral and maxillofacial surgeon Arne Geir Grønningsæter and oral physiologist Daina Fitins.
References
Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M, Cowley AW. Temporomandibular disorders and associated clinical comorbidities. Clin J Pain. 2011; 27: 268 - 274.
Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008; 359: 2693 - 2705.
Fillingim RB, Slade GD, Diatchenco L, Dubner R, Greenspan JD, Knott C, Ohrbach R, Maixner W. Summary of findings from the OPPERA baseline case-control study: implications and future directions. J Pain. 2011; 12: 102 - 7.
Bell FR, Borzan J, Kalso E, Simonnet G. Food, pain and drugs: Does it matter what pain patients eat? Pain. 2012; 153; 1993 - 196.
Haketa T, Kino K, Sugisaki M, Amemori Y, Ishikawa T, Shibuya T, Sato F, Yoshida N. Difficulty of food intake in patients with temporomandibular disorders. Int J Prosthodont. 2006; 19: 266 - 70).
Foreman PA. The changing focus of chronic temporomandibular disorders: management within a hospital-based, multidisciplinary pain center. N Z Dent J. 1998; 94: 23 - 31.
Miller DB. Clinical management of chronic TMD pain. Funct Orthod. 1998; 15: 35 - 9.
Rollman GB, Gillespie JM. The role of psychosocial factors in temporomandibular disorders. Cur Rev Pain. 2000; 4: 71 - 81.
Gameiro GH, da Silva Andrade A, Nouer DF, Ferraz de Arruda Veiga MC. How may stressful experiences contribute to the development of temporomandibular disorders? Clin Oral Investig. 2006; 10: 261 - 8.
Velly AM, Look JO, Carlson C, Lenton PA, Kang W, Holcroft CA, Fricton JR. The effect of catastrophizing and depression on chronic pain - a prospective cohort study of temporomandibular muscle and joint pain disorder. Pain. 2011; 152: 2377 - 2383.
Ahmed N, Poate T, Nacher-Garcia C, Pugh N, Cowgill H, Page L, Matthews NS. Temporomandibular joint multidisciplinary team clinic. Br J Oral Maxillofac Surg. 2014; 52: 827 - 830.
Zakrzewska JM. Differential diagnosis of facial pain and guidelines for management. Br J Anaesth. 2013; 111: 95 - 104.
Questions in parliament to the Minister of Health and Care Services. https://www.stortinget.no/no/Saker-og-publikasjoner/Sporsmal/Skriftlige-sporsmal-og-svar/Skriftlig-sporsmal/?qid=53932 https://www.stortinget.no/no/Saker-og-publikasjoner/Sporsmal/Skriftlige-sporsmal-og-svar/Skriftlig-sporsmal/?qid=53129
Bell RF. An integrated pain clinic model. Letter to the editor. Pain Medicine. 2015; May 29. doi: 10.1111/pme.12827. [Epub ahead of print]
Israel HA, Scrivani SJ. The interdisciplinary approach to oral, facial and head pain. J Am Dent Assoc. 2000; 131: 919 - 26.
https://helsedirektoratet.no/Sider/Nasjonal-faglig-retningslinje-for-utredning-og-behandling-av-TMD.aspx
Swedish Council on Medical Assessment (SBU). Methods of treating chronic pain. Report no. 177, 2006. https://www.sbu.se/en/Published/Yellow/Methods-of-Treating-Chronic-Pain/
Socialstyrelsen, guidelines for Oral physiology- pain and functional disorders of the mouth, face and jaw, 2011. https://www.socialstyrelsen.se/tandvardsriktlinjer/omriktlinjerna/omradeniriktlinjerna/bettfysiologi
https://www.uptodate.com/contents/temporomandibular-disorders-in-adults
Stegenga B, de Bont LG, de Leeuw R, Boering G. Assessment of mandibular function impairment associated with temporomandibular joint osteoarthrosis and internal derangement. J Orofac Pain. 1993; 7: 183 - 95.
Zigmond AS & Snaith RP, The hospital anxiety and depression scale, Acta Psychiatr Scand. 1983; 67: 361 - 70
Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One- and two-item measures of pain beliefs and coping strategies. Pain. 2003; 104: 453 - 469.
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RCD/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache. 2014; 28: 6 - 27.
Wilkes CH. Internal Derangements of the Temporomandibular Joint. Pathological Variations. Arch Otolaryngol Head Neck Surg. 1989; 115: 460 - 477.
Dimitroulis G. A new surgical classification for temporomandibular joint disorders. Int. J. Oral Maxillofac. Surg. 2013; 42: 218 - 222.
Rosén A, Feldreich A, Dabirian N, Ernberg M. Effect of heterotopic noxious conditioning stimulation on electrical and pressure pain thresholds in two different anatomical regions. Acta Odontol Scand. 2008; 66: 181 - 188.
Feldreich A, Ernberg M, Lund B, Rosén A. Increased beta-endorphin levels and generalized decreased pain thresholds in patients with limited jaw opening and movement-evoked pain from the temporomandibular joint. J Oral Maxillofac Surg. 2012; 70: 547 - 556.
Quartana PJ, Buenaver LF, Edwards RR, Klick B, Haythornthwaite JA, Smith MT. Pain catastrophizing and salivary cortisol responses to laboratory pain testing in temporomandibular disorder and healthy participants. J Pain. 2010; 11: 186 - 94.
Moen K, Hellem S, Geitung JT, Skartveit L. A practical approach to interpretation of MRI of the temporomandibular joint. Acta Radiolog. 2010; 51: 1021 - 7.
Badel T, Pavi?in IS, Zadravec D, Krapac L, Kern J. Osteoarthritic temporomandibular joint changes confirmed by magnetic resonance imaging. Reumatizam. 2012; 59: 15 - 21.
Ahmad M, Hollender L, Andersson Q, Kartha K, Orhbach R, Truelove EL, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 844 - 860.
Campbell LC, Riley JL 3rd, Kashikar-Zuck S, et al. Somatic, affective, and pain characteristics of chronic TMD patients with sexual versus physical abuse histories. J Orofac Pain 2000; 14:112.
Kvåle A, Skouen JS, Ljunggren AE. Discriminative validity of the Global Physiotherapy Examination-52 in patients with long-lasting musculoskeletal pain versus healthy persons. J Musculoskelet Pain. 2003; 11: 23 - 36.
DaSilva AF1, Shaefer J, Keith DA. The temporomandibular joint: clinical and surgical aspects. Neuroimaging Clin N Am. 2003; 13: 573 - 82.
Holmlund A, Lund B, Weiner CK. Discectomy without replacement for the treatment of painful reciprocal clicking or catching and chronic closed lock of the temporomandibular joint: a clinical follow-up audit. Br J Oral Maxillofac Surg. 2013; 51: 211 - 4.
Berge TI, Kubon B. Er artroskopi av kjeveleddet effektivt mot smerter og gapevansker? Nor Tannlegeforen Tid. 2012; 122: 670 - 5.
Holmlund A. Disc derangements of the temporomandibular joint. A tissue-based characterization and implications for surgical treatment. Int J Oral Maxillofac Surg. 2007; 36: 571 - 6.
Bjørnland T, Larheim TA. Diskectomy of the temporomandibular joint: 3-year follow-up is a reliable predictor for the long-term outcome. J Oral Maxillofac Surg. 2003; 61: 55 - 60.
Bjørnland T, Gjærum AA, Møystad A. Osteoarthritis of the temporomandibular joint: an evaluation of the effects and complications of corticosteroid injection compared with injection with sodium hyaluronate. J Oral Rehabil. 2007; 34: 583 - 589.
Møystad A, Mork-Knutsen BB, Bjørnland T. Injection of sodium hyaluronate compared to a corticosteroid in the treatment of patients with temporomandibular joint osteoarthritis: a CT evaluation. Oral Surg Oral Med Oral Pathol Endod. 2008; 105: 53 - 60
Holmlund A, Lund B, Weiner CK. Mandibular condylectomy with osteoarthrectomy with and without transfer of the temporalis muscle. Br J Oral Maxillofac Surg. 2013; 51: 206 - 10.
Loveless T, Bjornland T, Dodson TB, Keith DA. Efficacy of temporomandibular joint ankylosis surgical treatment. J Oral Maxillofac Surg. 2010; 68: 1276 - 82
Dragesund T, Råheim M. Norwegian psychomotor physiotherapy and patients with chronic pain: Patients' perspective on body awareness. Physiother Theory Pract. 2008; 24: 243 - 254.
Yu L, McCracken LM. Model and Processes of Acceptance and Commitment Therapy (ACT) for Chronic Pain Including a Closer Look at the Self. Curr Pain Headache Rep. 2016 Jan;20(2):12.
Corresponding author: Annika Rosén, Department of Clinical Dentistry, Division of Oral and Maxillofacial Surgery, University of Bergen, Bergen, Norway. E-mail: annika.rosen@uib.no
This paper has been peer reviewed.
Berge T, Schjödt B, Bell RF, Johansson A, Paulsberg A-G, Geitung JT, Rosén A. Assessment of patients with severe temporomandibular disorder in Norway - A multidisciplinary approach. Nor Tannlegeforen Tid. 2016; 126: 114-21.
Artikkelen er fagfellevurdert.
Artikkelen siteres som:
Berge T, Schjödt B, Bell RF, Johansson A, Paulsberg A, Geitung J, Rosén A. Assessment of patients with severe temporomandibular disorder
in Norway - a multidisciplinary approach. Nor Tannlegeforen Tid. 2016;126:114-21. doi:10.56373/2016-2-5