Acute dental pain II: pulpal and periapical pain
Acute dental pain most often occurs in relation to inflammatory conditions in the dental pulp or in the periradicular tissues surrounding a tooth, but it is not always easy to reach a diagnose and determine what treatment to perform. The anamnesis and the clinical examination provide valuable information, and a systematic approach is necessary.
This paper will focus on diagnosis and treatment of pulpitis, pulp necrosis and apical periodontitis, periodontal abscess and endodontic-periodontal lesions, pericoronitis and post-operative problems.
When the patient seeks the dentist suffering from acute dental pain, they expect that the dentist starts treatment at once and that the treatment should provide pain relief. In this situation many patients are fragile, anxious and nervous. If the dentist is able to manage emergency treatment of acute dental pain this will build confidence and trust between patient and dentist. However, often the dentist does not have sufficient time to carry out more time-consuming procedures. This paper provides a guide for rational emergency treatments. It describes how or whether the entire treatment or a less time-consuming pain relieving procedure should be carried out. The administration of local anesthesia, the role of antibiotics and analgesics is discussed.
Headlines | |
|---|---|
· |
Pain management and strategies for pain control are fundamental in care of acute conditions from the pulp or the periradicular tissues. |
· |
Drainage should always be obtained when swelling and pus formation occur in the soft tissue to diminishing the risk of infectious spread and pain relief. |
· |
The acute treatment should be based on the assessment of the risk for local or systemic spreading of infection. |
· |
Systemic antibiotics are usually not indicated in cases of a localized abscess and their role in pain reduction is limited. However, they have a definite role as a supplement in cases where drainage is not possible, if there is evidence of spreading infection or if the general health is affected. |
Clinical aspects of management of patients with acute pain originating from the pulp or the peripheral tissue of the tooth will be reviewed.
A frequent cause of tooth related pain is inflammation due to a localized entrapment of bacterial infection. Bacterial infections or bacterial products exposing the dental pulp will trigger a cascade of pathologic changes and cause purulent inflammation in the pulp tissue (pulpitis). Caries is the main reason for infection exposing the pulp, but it may also occur in teeth by fractures, cracks in the crown or open restoration margins (Figure1)

Figure 1. A molar with extensive crack trough crown and root providing a pathway to the pulp for bacteria and thereby inducing an inflammatory reaction in the pulp tissue. Extraction was performed due to the extent of the crack.
If severe irreversible inflammation occurs, this process will spread throughout the entire pulp space and cause pulp necrosis. With a pulp necrosis an infection will develop over time and bacteria will invade the pulp space. In the periapical tissues the host defence will develop an inflammatory reaction (apical periodontitis), due to the pulp infection. A high proportion of patients seeking emergency dental treatment have symptoms of pulpal or periapical disease [1]. Other acute dental conditions can develop from pathogens entrapped in periodontal pockets or adjacent to erupting teeth under the soft tissue flap (operculum) causing periodontal abscess or pericoronitis, respectively.
An inflammatory process will develop differently depending on the type and location of infection and the host's immune response. The type of process can be categorised as either an abscess or cellulitis. An abscess is a collection of pus and tissue swelling within the soft tissue. If the amount of pus increase the pressure in the tissue rise and an abscess may eventually perforate adjacent tissues and establish a fistula through the oral mucosa or skin allowing natural drainage of the infection and diminishing the risk of infectious spread.
In contrast to an abscess, cellulitis is a diffuse erythematous swelling and infection spreading in the connective tissue. Cellulitis is usually painful and may be accompanied by malaise and fever. The tissue spaces of the head and neck may facilitate the spread of pathogens and related inflammatory exudate within the fascial planes and in rare cases, if not properly handled, serious complications may occur and be potentially life-threatening [2].
Most of the acute dental inflammatory states develop spontaneously, but in conjunction with certain dental treatments there is a higher risk of inducing postoperative pain (flare-up).
All dental treatments should include a general medical and local dental anamnesis and a careful clinical examination, to establish the best possible basis for a diagnosis and treatment.
In an acute situation the dentist often has time constraints and thus special demands to the clinician's skill are required. The acute treatment should be based on location of the infection and consideration of the risk of its local or systemic spreading and the patient's general health.
Management of patients with acute dental pain
From a psychological perspective
Many patients are nervous or anxious prior to endodontic treatment of acute pain. The expectation of pain during or following treatment may be very strong particularly in highly anxious patients, and the pain may be triggered simply by touching the suspected tooth [3].
The increased reactivity derive partly from neurogenic inflammation (see chapter 1), leading to increased sensitivity and activity in otherwise inactive neurons, and is partly psychological in nature [4]. From a psychological perspective, the initial challenge for the dentist is to get the patient´s confidence, because the patient's assessment of the dentist's skill will be reflected in how painless the treatment per se can be performed.
Treatment of acute pain should include strategies based on information, distraction, relaxation or possibly hypnosis [3].
Preparing emergency treatment
Anesthetic considerations
Local anaesthesia can be administrated as infiltration or nerve block. In the maxilla, infiltrations are usually preferred because the bone is fairly porous and the liquid can infiltrate the bone.
In the mandible, the outer layer of cortical bone is thicker and a nerve block should be the first choice. Labial or lingual infiltrations alone are not effective for pulpal anesthesia in mandibular teeth [5].
Sufficient local anesthesia is essential, but can sometimes be difficult to achieve. It has been stated that for an inferior nerve block a single carpule will be sub-optimal in 30 - 80 % of cases with acute irreversible pulpitis [6]. Notably, the lack of pain relief in some patients may be due to prolonged onset. The onset of pulpal anesthesia usually occurs 10 - 15 min following inferior alveolar nerve block injection. However, in 20 - 30 % of the patients the time from the injection to pain relief may be longer, and in 10 % it may take up to 30 min before full effect is obtained [7].
In the literature there is no consensus for the beneficial effect of repeating a mandibular injection (in cases of absence of impact) to increase the volume of anesthetic liquid. Interestingly, lack of precision for placing the needle seems also to be of minor importance (within certain limits) and not evaluated to be essential for the effect [8]. However, there may be a few exception. The nervus mylohyoideus sometimes branches to the mandibular molars [9]. In order to include this within the anesthetic strategy, the needle should be placed either higher on the ramus or supplemented with an injection in the floor of the mouth.
A mandibular buccal infiltration using articaine (4 %) has been shown to provide an additive effect to mandibular block [10]. However, except for this there is no robust evidence in the literature to suggest that any of the routinely used anesthetics has a general distinguishing anesthetic effect.
Injection in acutely inflamed tissue should be avoided to prevent spreading of infection, and presence of inflammation decreases local anesthetic efficacy [11].
Preoperative pain medication with non-steroidal anti-inflammatory medication (NSAIDs) 1 hour before administrating anesthetics has been shown to increase the efficacy in patient with acute pulp inflammation [12]. If the sensibility test after prolonged observation still reveals sensitivity, it is advised to proceed with supplemental techniques, such as intraligamentary or intrapulpal injection (box 1 and 2).
Box 1
Intraligamentary injection
The periodontal ligament injection is used as either a method of obtaining primary anesthesia or as a supplement to failed infiltration or block techniques.
In mandibular posterior teeth with irreversible pulpitis, an intraligamentary injection may be a good supplement .
Benefits of intraligamentary injection are: reduced dose, less soft tissue anesthesia and fast on-set.
Injection time is about 20 sec. and the effect is usually obtained after 30 sec.
The pain associated with intraligamentary or palate injection may be reduced, if syringes with pre-dosed measured volumes (Parojet) or computer-controlled pre-programmed speed set-up (eg. The wand, or SleeperOne Analge-Ject), are used instead of conventional syringes.
Box 2
Intrapulpal injection
Intrapulpal injection is the very final attempt to obtain pain relief. It is a painful procedure and should only be carried out in complete compliance with the patient.
A perforation to the pulp is obtained with a small bur.
The pulp should be bathed in a little local anesthetic solution before introducing the needle into the pulp chamber
The injection should be performed under pressure (0.2 ml).
The mechanical pressure during injection of the liquid is of importance. A few studies have shown that the type of medicament apparently is of minor importance since injection of saline was as effective as anesthetic liquid.
Symptomatic pulpitis
Diagnostic considerations
When patients arrive with pain, the pain profile may not correspond with the actual presence of pulp inflammation [13]. Based on subjective and objective findings pulpitis is divided into two clinical diagnoses: irreversible pulpitis and reversible pulpitis. In reversible pulpitis a local inflammation should be able to resolve and the pulp return to normal following appropriate management of the cause of the condition.
In irreversible pulpitis, on the other hand, the dental pulp is severely inflamed and damaged beyond repair. In the acute phase it is associated with spontaneous burst of intense pain that tend to linger for minutes or more.
The clinical diagnosis is mainly based on anamnesis and clinical symptoms such as degree/characteristic of pain and signs associated with pulpal inflammation. The needed diagnostic considerations are outlined in Table 1.
Pulp condition |
||
|---|---|---|
Diagnostic factors |
Reversible pulpitis |
Irreversible pulpitis |
Spontaneous toothache |
No |
Yes |
Sensitivity (cold and electricity) |
Yes |
Yes |
Prolonged sensitivity to cold |
No |
Yes |
Prolonged sensitivity to heat |
No |
Yes |
Pain relief from cold |
No |
Possible |
Swelling |
No |
No |
Increased mobility |
No |
Possible |
Tenderness to percussion |
No |
Yes |
Excessive bleeding of the pulpLarge potential of hemostasis after pulp exposure |
NoYes |
PossibleNo |
Radiographic signs (periodontal ligament) |
No |
Possible |
Treatment principles
Caries is the most frequent reason why dentists perform root canal treatment [14]. There is a correlation between the depth of caries lesion and the degree of inflammation in the pulp [15]. It seems to be crucial for the prognosis of preserving pulp vitality if caries excavation can be performed without pulp communication [16].
If the pulp is exposed due to a deep caries lesion, pulpotomy or pulpectomy, should be performed and this is most reliable treatment to obtain pain relief [17].
Prescribing of systemic antibiotics for symptomatic irreversible pulpitis will not provide any pain relief [18]. The infection is located inside the hard dental tissues or in superficial parts of the necrotized pulp tissue, where antibiotics from the bloodstream cannot reach it.
Pulpotomy
The aim of a pulpotomy is to remove the inflamed coronal pulp tissue from the pulp chamber without penetrating into the radicular pulp tissue. The pain relieving effect is most probably due to a removal of the source of inflammation and drainage with a concomitant reduction in local tissue pressure and concentration of inflammatory mediators. Pulpotomy leads to pain relief in 90 % of treated cases [17, 19.
The use of a diamond drill with a non-cutting tip is very suitable to remove the roof of the pulp chamber after access (Figure 2), and a slowly rotating bur is used to remove the coronal pulp tissue.

Figure 2. A diamond bur with a non-cutting tip mounted in a high-speed handpiece is useful for removing the roof and finishing the walls of the pulp cavity during access preparation. However, remember to stay within the outlines of the walls of the pulp chamber. In this mandibular molar over-extention has started to occur (arrow).
Irrigate with plenty of NaOCl to cleanse the area and stop the bleeding. If bleeding still occurs use an aqueous mixture of calciumhydroxide or a pellet of 3 % hydrogen peroxide on the canal orifices until the bleeding stops.
Using local sedative or antibacterial dressings, such as eugenol, camphorated phenol or steroids have previously been used and regarded as crucial for pain relief but this effect has not been shown in comparative studies [17].
The thickness of the temporary restoration is of importance when multiple endodontic visits are performed. The temporary filling should at least be 4 mm thick to maintain a bacteria tight sealing [20].
It is important that the patient is informed that the dental treatment is not finished and that a new appointment is needed to complete the treatment and ensure that the pain does not reappear.
Pulpectomy
Clinically it is difficult to determine the extent of the pulpal inflammation. Therefore, performance of pulpectomy and complete removal of the pulp tissue is 'standard of care' treatment of irreversible pulpitis, if there is no time restrictions [16].
It is fundamental that the pulpectomy is performed under aseptic conditions. As soon as the pulp chamber is exposed, rubber dam should be used for isolating the tooth from oral and salivary contamination. Introducing microorganisms to the root canal increase the risk of postoperative pain and reduce the prognosis for the treatment.
After the chemomechanical treatment of the root canal system the root filling can either be performed during the same appointment or after an inter-appointment dressing with calciumhydroxide.
Pulp necrosis and symptomatic apical periodontitis
Considerations of local or systemic spreading of infection
Apical periodontitis is an inflammatory disease in the periradicular tissue of the tooth caused by microorganisms (mainly bacteria) infecting the necrotic root canal system.
The intensity of inflammatory response will depend on the quantitative (number) and qualitative (virulence) nature of the microorganisms and the host inflammatory response. A swelling within the soft tissue may appear, that can be either localized (abscess) or diffuse (cellulitis).
In most cases apical periodontitis is related to a specific tooth and there is no signs of spreading of the infection. In rare cases, however, the infection may spread through the connective tissue and result in life-threatening complications such as Ludwig's angina or brain abscess.
Treatment principles
The elimination of local microbial factors by chemomechanical debridement of the root canal system should be performed if there is enough time [16].
Caries and fillings at risk of leakage should be removed and the root canal treatment should be performed under aseptic conditions using rubberdam to avoid additional microbes entering the root canal system.
It is possible to create drainage from the periradicular tissues through the root canals and to reduce localized tissue pressure by exploring the apical foramen with a thin file (size 10 - 15). The root canal system should be filled with calciumhydroxide and the access cavity sealed with a temporary filling.
The first-line treatment for teeth with symptomatic apical periodontitis should be establishment of adequate drainage either through the pulp chamber (Figure 3), by incision and drainage or by extraction. Drainage facilitates the evacuation of pus, allow decompression and consequently provide pain relief. The pulp chamber should not be left open for drainage. The microbial flora in the canal will change making disinfection more difficult and, furthermore, it may increase the risk of subsequent flare-up [21].
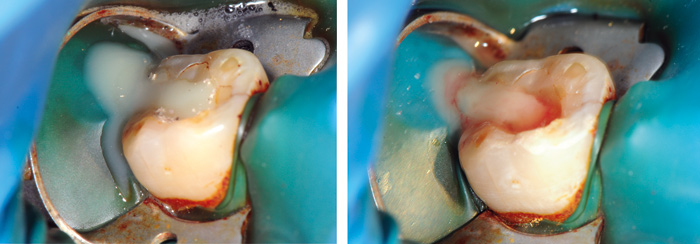
Figure 3. Molar with pulp necrosis and apical pariodontitis showing spontanous drainage of pus through the pulp chamber after access preparation. After a while the pus fills the cavity with signs of bloody exudate.
When a mature, fluctuating abscess is localized, it should be incised and drained through the mucosa by a minor surgical procedure. In most cases, a drain placed in the incision for 24 - 48 hours will allow for adequate drainage.
In situations with limited time, performing an access cavity preparation, providing an opening to the pulp chamber and placing a temporary filling, gives pain relief for a substantial proportion of patients [16]. However, this strategy should not be attempted in patients with swelling and or pus formation.
Extraction of the diseased tooth is the simplest and most effective pain relieving method as it removes the source of infection and drains the pus and should always be considered in cases with extensive loss of coronal tooth substance and questionable restorability.
Antibiotics and painkillers
Prescription of antibiotics should always be preceded by a benefit risk analysis on an individual basis. Antibiotics are usually not indicated in cases of a localized abscess and its role in pain reduction is limited [22]. The pain associated with acute apical periodontitis is best treated with analgesics. No other known medicaments have the potential to reduce the pain [23]. NSAIDs or, if contraindicated, paracetamol should be prescribed [24]. NSAIDs and paracetamol can be used effectively in combination in a two-hour dosing schedule. If this does not provide sufficient pain relief opioid analgesics may be required.
Systemic antibiotics have a definite role as a supplement to clinical procedures in cases where drainage is not possible and there is evidence of spreading infection (trismus, cellulitis, lymph node involvement, pain during swallowing) or systemic involvement, where the general health is affected e.g. the patient being feverish (malaise) or if a swelling rapidly increases.
The choice of antibiotic is influenced preliminary by the stage of infection development and the ability of the patient to take the antibiotic - medical conditions or allergy.
First-line antibiotics is phenoxymethylpenicillin (PcV) and if insufficient metronidazol should be added. In case of allergy clindamycin is the first choice of treatment [25]
With appropriate acute treatment symptom relief can be expected within two-three days and after five days a high proportion of teeth will be asymptomatic [26].
Post-operative pain after endodontic treatment
Endodontic flare-up is defined as strong pain with or without swelling that occurs after the initiation or continuation of root canal treatment. The reported incidence varies from 0 %-12 % with an average of 8.4 % [27].
Several factors may be associated with the phenomena, mechanical as well as bacteriological: Preparation beyond apical terminus, dentin chips and/or infected pulp tissue pushed into the periapical area, overextension of root canal filling, and ecologic changes during endodontic therapy resulting in selective growth of certain bacterial species inside the root canal [28, 29].
In the presence of suppuration, drainage of exudate is the most effective method for reducing pain and swelling. In some occasions the exudate cannot or will not drain through the root canal and surgical intervention by a soft tissue incision may be necessary.
If bacteria are allowed to persist in the root canal system after endodontic treatment, and not excluded from nutritive then they will continue to be active and this may result in pain. In such cases retreatment with a surgical approach may be considered. If there is vertical root fracture fractured tooth should be extracted (Figure 1).
Periodontal abscess and endodontic-periodontal lesion
Diagnostic considerations
Endodontic-periodontal lesions may be a diagnostic challenge to the clinician [30], but it is of vital importance to make a correct diagnosis so that the appropriate treatment can be provided. It is important to diagnose potential contributing factors such as root fractures, root resorptions, perforations, and dental malformations that may play important roles in the development, progression and prognosis of endodontic-periodontal lesions. The recognition of pulp vitality is essential for differential diagnosis and treatment decision related to inflammatory lesions in the marginal and apical periodontium. Acute exacerbation from a periapical abscess may drain/fistulate through the periodontal ligament into the gingival sulcus (Figure 4). This condition can mimic the presence of a periodontal pocket or abscess
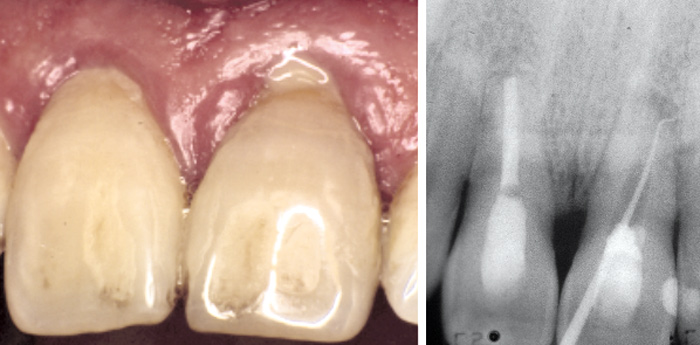
Figure 4. Tooth 21 with an endodontic-periodontal lesion showing spontantaneous drainage of pus from the periodontal pocket. The radiographs showing the sinus tract traced with gutta-percha point.
Treatment principles
Periodontal lesions of endodontic origin heal following endodontic treatments. However, the prognosis of the treatment is less favourable if the patient suffers from a general marginal periodontal problem.
The initial management of a periodontal abscess involves pain relief and control of the infection. This can be encouraged by gentle irrigation with saline and scaling of the pocket whilst massaging the soft tissues. With a history of recurrent periodontal abscesses and significantly compromised periodontal support extraction of the tooth should be considered.
Primary periodontal disease with secondary endodontic involvement and true combined endodontic-periodontal diseases require both endodontic and periodontal therapies.
A summary of the different conditions is seen in Table 2.
Aetiology |
Pulp-status |
Treatment |
Prognosis |
|---|---|---|---|
Endodontic |
Necrotic/infected |
Endodontic |
Good |
Periodontal |
Vital |
Periodontal |
Questionable |
Endodontic and periodontal |
Necrotic/infected |
Endodontic and periodontal |
Poor |
Pericoronitis and aspects involving third molar removal
Diagnostic considerations
The indications for third molar surgery have been discussed throughout the years and have been a topic of controversy. There is not enough evidence to support prophylactic removal of third molars [31], and the consensus today is that third molars should be removed only if they repeatedly cause problems or if there is a risk of future damage to neighbouring teeth.
This may occur when the third molar lack space in the mandible during eruption, and is a common developmental problem. The third molar may be partially or completely impacted against adjacent tooth, the mandible ramus and surrounding soft tissue. If bacteria gain access into the follicular space through an opening in the overlying gingiva, an inflammation in the surrounding tissue, pericoronitis, will develop.
Symptoms involved in pericoronitis are pain, swelling of soft tissue and alveolar osteitis.
Treatment principles in cases of symptoms
Local treatment, such as rinsing with sodium chloride in the soft tissue pocket, instructions of improved brushing technique and mouth rinsing with an antibacterial medium, is the first step, and may slow down the infection. Grinding on the opposing tooth may be considered, if the patient experience pain when biting or if the opposing tooth will traumatize the swollen operculum further. If the condition gets worse, the patient may develop trismus, lymph node involvement, pain during swallowing and feel generally unwell with fever.
If an abscess develops, within a fibrin capsule, it has to be drained by an incision.
Recurrent pericoronitis is an indication for third molar surgery, but it is important to treat the infection before the surgical removal, to reduce the risk for spreading of the bacterial infection.
Antibiotics and painkillers
Antibiotics should be considered where drainage is not possible, there is evidence of spreading infection or systemic involvement. First choice of antibiotics is phenoxymethylpenicillin (PcV) and if that is not enough metronidazol can be added. In case of allergy clindamycin is the first choice but can also be used when a broader spectrum antibiotic is necessary.
NSAID/paracetamol should be prescribed separately or in combination. If the patient does not show improvement NSAID/paracetamol in combination with opioid could be used.
In case of suspected diffuse spreading into deeper spatiums (flegmone, Ludwigs angina), the patient needs to be treated in the hospital. Signs of this condition are swollen mouth floor, trismus, dysfagi and dyspné with high frequent breathing (stridor) and fever. The patient must immediately be referred to the hospital for treatment where i.v. antibiotics and drainage of the abscess will be performed. In some cases the condition can be life threatening.
Postoperative pain and flare-up after surgery
Oral surgery is associated with postoperative pain, swelling and trismus. These symptoms are expected within the first three postoperative days, but if they are not treated well they are considered as complications.
Pre-emptive analgesics with paracetamol or NSAIDs can increase the time before pain onset and decrease the need of postoperative analgesics [32].
Postoperative pain may develop to persistent pain and new research point at neuro-inflammation as a cause. In the clinical situation it is therefore important to reduce the acute pain, since further progress of pain can be more difficult to treat [33]. Full dose of analgesics is an important factor; to reduce the pain signals and minimize the risk of prolonged or persistent pain [34].
Complications to the surgical procedure occur in the intra- or postoperative phases and include alveolitis with persistent pain, infection, bleeding and paraesthesia. The incidence of complications varies from 4.6 % to 30.9 % [35].
Alveolitis, sicca doloroses (dry socket) is one of the most frequent complications after mandibular third molar surgery and is characterised by pain setting in 2 - 3 days after surgery. After extraction, it is important to let a blood clot develop in the alveolus to reduce the risk for dry socket. An empty socket, which is partially or totally devoid of blood clot with exposed bone, is extremely painful. Other symptoms may be halitosis and bad taste in the mouth. Treatment is usually symptomatic and analgesics and/or local anaesthetics are needed until the pain fades away after up to 3 - 4 weeks. Rinsing with sterile sodium chloride and a tamponade with a mixture of lidocain- and corticosteroid paste may be used initially and can ease the pain. The tamponade should not be left in the socket for more than 24 hours.
References
Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993; 124: 115 - 21.
Skaug N, Berge TI, Bårdsen A. Akuta infektioner. Tandläkartidningen. 2005; 97(1): 54 - 62.
Eli L, Svensson P. The multidimensional nature of pain. In: Bergenholtz G, Hørsted-Bindslev P, Reit C, eds. Textbook of endodontology. Oxford: Wiley-Blackwell, 2010; 277 - 87.
Craig KD. Emotional aspects of pain. In: Wall PD, Melzack R, eds. Textbook of pain 2nd ed. London: Churcill Livingstone; 1989.
Yonchak T. et al. Anesthetic efficacy of infiltrations in mandibular anterior teeth. Anesth Prog. 2001. 48: 55 - 60.
Hargreaves KM, Keiser M. Local anesthetic failure in endodontics: Mechanisms and management. Endodontic Topics. 2002; 1: 26 - 39.
Reader A, Nusstein J. Local anesthesia for endodontic pain. Endodontic Topics. 2002; 3: 14 - 30.
Hannan L. et al. The use of ultrasound for guiding needle placement for inferior alveolar nerve blocks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87: 658 - 65.
Matthews R, et al. Articaine for supplemental buccal mandibular infiltration anesthesia in patients with irreversible pulpitis when the inferior alveolar nerve block fails. J Endod. 2009; 35: 343 - 6.
Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012; 38: 421 - 5.
Modaresi J, Dianat O, Soluti A. Effect of pulp inflammation on nerve impulse quality with or without anesthesia. J Endod. 2008; 34: 438 - 41.
Noguera-Gonzalez D et al. Efficacy of preoperative ibuprofen on the success of inferior alveolar nerve block in patients with symptomatic irreversible pulpitis: a randomized clinical trial. Int Endod J. 2013; 46: 1056 - 62.
Johnson RH, Dachi SF, Haley JV. Pulpal hyperemia - a correlation of clinical and histologic data from 706 teeth. J Am Dent Assoc. 1970; 81: 108 - 17.
Bjørndal L, Laustsen MH, Reit C. Root canal treatment in Denmark is most often carried out in carious vital molar teeth and retreatments are rare. Int Endod J. 2006; 39: 785 - 90.
Bjørndal L, Ricucci D. Pulp inflammation: From the Reversible Inflammation to Pulp necrosis during caries progression. In: Goldberg M. (ed). The Dental Pulp Biology, Pathology, and Regenerative Therapies. Berlin Heidelberg: Springer-Verlag. 2014; 125 - 39.
Bjerkén E, Wennberg A, Tronstad L. Endodontisk akutbehandling. Tandläkartidningen. 1980; 6: 314 - 9.
Hasselgren G, Reit C. Emergency pulpotomy: pain relieving effect with and without the use of sedative dressings. J Endod. 1989; 15: 254 - 6.
Nagle D, et al. Effect of systemic penicillin on pain in untreated irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90: 636 - 40.
Asgary S, Eghbal MJ. A clinical trial of pulpotomy vs. root canal therapy of mature molars. J Dent Res. 2010; 89: 1080 - 5.
Beach CW, et al. Clinical evaluation of bacterial leakage of endodontic temporary filling materials. J Endod. 1996; 22: 459 - 62.
Seltzer S, Naidorf IJ. Flare-ups in endodontics: I. Etiological factors. 1985. J Endod. 2004; 30: 476 - 81; discussion 475.
Cope A, et al. Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults. Cochrane Database Syst Rev. 2014; 6: CD010136.
Henry M, Reader A, Beck M. Effect of penicillin on postoperative endodontic pain and swelling in symptomatic necrotic teeth. J Endod. 2001; 27: 117 - 23.
Hargreaves K, Abbott PV. Drugs for pain management in dentistry. Aust Dent J. 2005; 50(Suppl 2): 14 - 22.
Larsen T, et al. Anvendelse af antibiotika i tandlægepraksis. Tandlægebladet. 2013; 117: 386 - 97.
Gilmore WC, et al. A prospective double-blind evaluation of penicillin versus clindamycin in the treatment of odontogenic infections. J Oral Maxillofac Surg. 1988; 46: 1065 - 70.
Tsesis I, et al. Flare-ups after endodontic treatment: a meta-analysis of literature. J Endod. 2008; 34: 1177 - 81.
Siqueira JFjr. Microbial causes of endodontic flare-ups. Int Endod J. 2003; 36: 453 - 63.
Trope M. Relationship of intracanal medicaments to endodontic flare-ups. Endod Dent Traumatol. 1990; 6: 226 - 9.
Al-Fouzan KS. A new classification of endodontic-periodontal lesions. Int J Dent. 2014; 2014: 919173.
Steed MB. The indications for third-molar extractions. J Am Dent Assoc. 2014; 145: 570 - 3.
Joshi A. Parara E, Macfarlane TV. A double-blind randomised controlled clinical trial of the effect of preoperative ibuprofen, diclofenac, paracetamol with codeine and placebo tablets for relief of postoperative pain after removal of impacted third molars. Br J Oral Maxillofac Surg. 2004; 42: 299 - 306.
Juhl GI, et al. Central sensitization phenomena after third molar surgery: a quantitative sensory testing study. Eur J Pain. 2008; 12: 116 - 27.
Weil K, et al. Paracetamol for pain relief after surgical removal of lower wisdom teeth. Cochrane Database Syst Rev. 2007: CD004487.
Bui, C.H., E.B. Seldin, and T.B. Dodson, Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg, 2003. 61(12): 1379 - 89.
Corresponding author: Peter Jonasson, e-post: peter.jonasson@odontologi.gu.se
This paper has been peer reviewed.