Dental erosion
Erosive tooth wear is a multifactorial cumulative lifetime process, which may lead to tooth surface loss. Acids of intrinsic and extrinsic origin are the main etiological factors. This paper has its focus on preventive measures and minimally invasive restorations. The application of high fluoride, time of tooth brushing as well as the intake of erosive foodstuffs or beverages should be optimised. Sealing of the tooth surfaces and small composite fillings are minimally invasive treatments of choice for erosive lesions.
Dental erosion is defined as a loss of tooth substance by chemical processes not involving bacteria (1). Erosion may be caused by intrinsic as well as by extrinsic factors.
The early signs of facial enamel erosion are a smooth silky-shining glazed surface with the absence of perikymata. In the more advanced stages further changes in the morphology can result in further flattening of the surface or development of a concavity in the enamel, the width of which clearly exceeds its depth. Undulating borders of the lesion are possible. Typically, it is an intact border of enamel along the oral and facial gingival margin. The reason for the band of preserved enamel could be due to some plaque remnants, which would act as a diffusion barrier for acids (2), or due to the acid neutralizing effect of the sulcular fluid, which has a pH between 7.5 and 8.0 (3). The initial features of erosion on oral and occlusal surfaces are the same as described above. The enamel has a glazed appearance. Further progression of occlusal erosion leads to a rounding of the cusps, grooves on the cusps and incisal edges, and restorations rising above the level of the adjacent tooth surfaces. In severe cases the whole occlusal morphology of the tooth disappears. The following index characterizes the morphological features:
Grading of facial surfaces
Grade 0: No erosion. Surface with a smooth, silky-shining appearance, absence of developmental ridges possible.
Grade 1: Loss of surface enamel. Intact enamel found cervical to the lesion. Concavity in enamel, the width of which clearly exceeds its depth, thus distinguishing it from toothbrush abrasion. Undulating borders of the lesions are possible.
Dentin is not involved (Fig. 1).

Fig. 1. Facial aspect of maxillary incisors showing weak (grade1, no involvement of dentin, tooth 11) and advanced (grade 2, involvement of dentin, tooth 21) erosion. Note the smooth silky-shining glazed surface and absence of perikymata but mostly intact border of enamel along the gingival margin.
Grade 2: Involvement of dentin for less than one half of the tooth surface. (Figs. 1, 2, 3).

Fig. 2. Tooth 21 shows an erosive defect grade 2 (involvement of dentin) on the facial surface. Note: Intact enamel along the gingival margin.

Fig. 3. Facial surfaces of the teeth 13, 14 with erosion grade 2.
Grade 3: Involvement of dentin for more than one half of the tooth surface.
Grading of oral and occlusal surfaces
Grade 0: No erosion. Surface with a smooth, silky-shining appearance. Absence of developmental ridges possible.
Grade 1: Slight erosion, rounded cusps, edges of restorations rising above the level of adjacent tooth surface, grooves on occlusal aspects. Loss of surface enamel. Dentin is not involved (Fig. 4).

Fig. 4. Occlusal erosion on tooth 15 and 16: Slight erosion, rounded cusps and grooves are characteristic for erosion grade 1 (tooth 15), whereas the involvement of dentin starting in the center of the cusps is typical for an erosion grade 2 (tooth 16).
Grade 2: Severe erosion, more pronounced signs than in grade 1. Dentin is involved (Figs. 5 – 9).

Fig. 5. Advanced erosion grade 2 on occlusal surface of tooth 35, 36.

Fig. 6. Severe occlusal erosion on primary molars 84 and 85. Already the permanent tooth 46 shows initial signs of erosion in the center of the cusps.

Fig. 7. Severe occlusal erosion on primary teeth 63 and 64. Plaque disclosing agent shows involvement of dentin.

Fig. 8. Oral erosion with involvement of dentin (grade 2) of the teeth 11, 21.

Fig. 9. Teeth 46, 47: Occlusal erosion with involvement of dentin. The edges of the amalgam restorations are rising above the level of the adjacent tooth surface (from ref. 12).
Erosive lesions have to be clearly distinguished from wedge-shaped defects. There is evidence that incorrect toothbrushing techniques may traumatise these tissues and lead to gingival recession with root surface exposure and cervical wedge-shaped defects often called toothbrush abrasions (4). In this context it should be mentioned that physical loading during interocclusal activities has also been discussed as one possible factor contributing to the formation of wedge-shaped defects. While true erosion is mainly caused by the action of acids and assisted by abrasion or attrition, wedge-shaped defects are primarily caused by abrasion (and occlusal stress) and only secondarily aggravated by acid softening of the hard tissue. Since the etiology as well as the prevention of wedge-shaped defects are different from those of erosive lesions, it is important that the dentist is able to distinguish between these conditions.
Prevention
When dental erosion is clinically detected or when there is indication of an increased risk, detailed patient assessment should be undertaken. A very important part is case history taking. However, chair-side interviews are generally not sufficient to determine dietary habits leading to erosion because the patients may be unaware of their acid ingestion. It is therefore advisable to have such patients record in writing their complete dietary intake for four consecutive days (Table 1). The time of day and quantity of all ingested food and beverages, including dietary supplements, should be recorded. Both weekdays and weekends should be included, as dietary habits during weekends may be considerably different from those during weekdays. This dietary and behaviour record should be sent to the dentist prior to the next appointment. The dentist should determine the erosive potential of the different acidic food items and drinks, the frequency of ingestion during main meals and snacks followed by an estimation of the daily acid challenge. It has also to be taken into account possible intrinsic acid exposure. As not all possible risk factors are recorded during these four days the patient should be questioned specifically and examined using the information provided in Table 2. Based on these analyses, a useable preventive program may be suggested to patients on an individual basis (Table 3). The goal of this program is to reduce acid exposure by decreasing the frequency of ingestion of potentially harmful drinks and foodstuffs as well as minimising contact time by rapid consumption rather than sipping or swishing or by controlling reflux/vomiting. The patient’s fluoride regime should be optimised. As discussed, various pathological processes cause the degradation of tooth substance. Erosion, attrition and abrasion often occur simultaneously, even though one of these factors may be predominant. When giving preventive instructions, all the causative components must be taken into consideration. Other behaviours that either stimulate salivary flow such as chewing gum or directly help to neutralise acids such as rinsing with sodium bicarbonate may counteract the destructive effects of dietary acids (5). Patients suffering from intrinsic erosions need, depending upon the cause, further care such as psychological therapy, antacida or even surgical intervention.
Day 1, Date: 06.06.2005 | ||
|---|---|---|
Time |
Foods/beverages |
Oral hygiene |
6,3 |
Yoghurt, 1 apple, honey, coffee with milk |
Toothbrushing immediately afterwards |
9,3 |
300 ml orange juice, sip-wise |
|
13,0 |
Cooked whole potatoes, cheese, salad with french dressing, herb tea and 1 apple |
Toothbrushing immediately afterwards |
16,2 |
300 ml orange juice, sip-wise |
Toothbrushingimmediately afterwards |
19,0 |
Mixed salad with french dressing, bread and herb tea |
|
20.00 – 21.00 |
300 ml orange juice, sip-wise |
|
22,0 |
1 orange |
|
23,0 |
Toothbrushing |
|
– |
Case history (medical and dental). |
|
– |
Detection of the main non-carious hard tissue lesions (site specific distribution) |
|
– |
Record of dietary intake over four days (estimation of the erosive potential)Specific factors which are seldom recorded as the patient may not be aware of. |
|
Diet: |
Sport drinks, herb teas, acidic candies, alcohol, effervescent vitamin C tablets etc. |
|
Gastric symptoms: |
Vomiting, acid taste in the mouth and gastric pain (especially when awakening), stomach ache, any sign of anorexia. |
|
Drugs: |
Alcohol, tranquillizer, antiemetics, antihistamins, lemonade tablets. (Replacement of acidic drugs or saliva reducing drugs is possible.) |
|
– |
Determination of flow rate and buffering capacity of saliva. |
|
– |
Oral hygiene habits. |
|
– |
Occupational exposure to acidic environments. |
|
– |
X-ray therapy of the head area. |
|
– |
Study models and/or photographs to assess further progression. |
|
– |
Avoid toothbrushing immediately after acid intake. Instead, rinse with a fluoride containing mouthrinse or with water. |
– |
Apply fluoride before the erosive challenge. |
– |
Use high concentrated topical fluoride periodically (slightly acidic formulations are preferable as they form with a higher rate a protective CaF2-layer on the tooth surface). |
– |
Reduce acid exposure by reducing the frequency (main meals only), and contact time of acids. |
– |
Do not hold or swish drinks in your mouth. |
– |
Finish meal with something «neutralising» (rich in Ca/P) such as cheese. |
– |
After acid intake stimulate saliva flow with chewing gum. |
– |
Refer the patient to a gastroenterologist and/or a psychologist (patients with intrinsic erosion). |
Acid-eroded enamel is more susceptible to abrasion and attrition than intact enamel. The thickness of the softened enamel that is removed after different abrasion procedures varies in different investigations depending on experimental conditions (for a review see 6). It appears that highly concentrated fluoride gels showed the best protection against further erosion/abrasion (7 – 9).
Experiments
In our own experiments we compared the impact of different fluoride procedures on the prevention of toothbrush abrasion of softened enamel when applied before softening. Softening was made in vitro with 0.1 M citric acid (pH 3.5) during 3 min. All runs were performed in which 4 slabs per run were attached to intraoral appliances. After exposing for 60 minutes to the oral milieu, the samples were brushed in situ for 15 s with a medium abrasive toothpaste and the loss of tooth substance was determined (Fig. 12). Toothbrush abrasion was lowest using the slightly acidic sodium/amine fluoride gel for 1 min before softening the enamel compared to all the other experimental groups (p<0.05). This could be due to some incorporation of material into and/or deposition of material on the enamel, most probably as a CaF2-like material (7, 8). There was no significant protecive effect in our experiment when Solidox Syreblokk® (Lilleborg as) was used. For individuals with a high risk for erosive tooth wear and with active erosion we suggest to postpone tooth brushing at least for one hour after consuming erosive foodstuffs or beverages in order to minimise enamel loss. Another possibility is the application of fluoride before the erosive attack (Fig. 12). For patients prone to caries, the risk of enhancing the progression of carious lesions by postponing tooth brushing may be too high because of the rapid decrease in plaque pH after ingestion of sugar-containing foods or beverages. Measures that would be both beneficial for erosion and caries would be rinsing with fluoride solutions to enhance remineralisation and chewing sugarless gum to stimulate the secretion of saliva.
Minimally invasive treatment
Early diagnosis of the process is a prerequisite to start preventive measures and to prevent every restoration. In no case may early diagnosis be an excuse for a restoration. The initiation of restorative treatment has to depend on individual circumstances and the perceived needs and concern of the patient.
The very first minimally invasive measure is the sealing of the tooth surface. In a study (10) the sealer/bonding products «Seal and Protect» and «Optibond Solo» were applied each to extracted teeth and subjected to 3 000 cycles in an erosion/abrasion wear machine. The amount of wear measured on the unprotected teeth was 243 m whereas on the protected surfaces it measured 24.8 m for «Seal and Protect» and 1.4 m for «Optibond Solo». It was concluded that both products protected the teeth in this wear regime and the technique could be used clinically for patients. Our own clinical experience shows an obvious decrease of hypersensitivity of erosive damaged teeth after sealing. However, the sealing procedures have to be repeated periodically.
Occlusal erosions typically show grooves on occlusal aspects and edges of restorations rising above the level of adjacent tooth surfaces. These grooves show a prolonged time of a depressed pH value after an acid attack (unpublished observation) which will lead to further progression of the erosive process at this site. In such cases minimally invasive composite fillings are able to protect the affected region (11). Conventional glass-ionomer cements are not recommended as permanent restorations because of their disintegration in acidic conditions (12). Advanced destructions will need more extensive restorations made of composite, ceramic veneers or even onlays or crowns. In all cases, the preparations have to follow the principles of minimally invasive treatment. It has to be kept in mind that the causes of the lesions have to be detected in order to stop the disease. Otherwise, the erosive process will further destroy tooth substance (Fig. 9 – 11).

Fig. 10. Minimally invasive treatement: The grooves of the molar of figure 9 were filled with composite, after the cause (regurgitation) was treated (from ref. 12).

Fig. 11. The occlusal surface of tooth 36 was restored with composite without treatment of the cause which was regurgitation. Progression of the erosion around the filling is clearly visible.
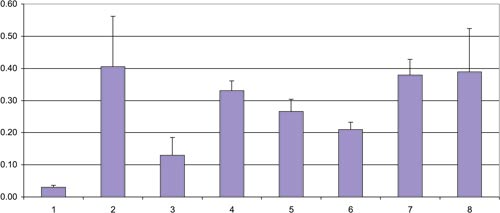
Fig. 12. Mean loss of polished enamel in micrometers after 15 s toothbrushing in situ (in part from ref. 11).
1) no softening, no fluoride (control 1); 2) softening, no fluoride (control 2); 3) sodium/amine fluoride gel (Elmex gel, 12 500 ppm F-) for 60 s before softening; 4) stannous fluoride (Emofluor, 1000 ppm F-) for 60 s before softening; 5) rinsing in situ with a sodium/amine fluoride rinsing solution (Elmex red rinsing solution, 250 ppm) for 30 s before softening; 6) rinsing in situ with a stannous/amine fluoride rinsing solution (Meridol rinsing solution, 250 ppm) for 30 s before softening; 7) application of NaF gel (Binaca, 12 500 ppm F-) for 60 s before softening; 8) application of stannous fluoride (Solidox Syreblokk, ~1100 ppm F-) for 60 s before softening.
References
1. Zipkin J, McClure FJ. Salivary citrate and dental erosion. J Dent Res 1949; 28: 613 – 26.
2. Schweizer-Hirt CM, Scheit A, Schmid R, Imfeld T, Lutz F, Mühlemann HR. Erosion und Abrasion des Schmelzes: Eine experimentelle Studie. Schweiz Monatsschr Zahnmed 1978; 88: 497 – 529.
3. Stephen K, McCrossan J, Mackenzie D, Macfarlane CB, Speirs CF. Factors determining the passage of drugs from blood into saliva: Br Dent Clin Pharmacol 1980; 9: 51 – 5.
4. Brady JM, Woody RD. Scanning microscopy of cervical erosion. J Am Dent Assoc 1977; 94: 726 – 9.
5. Amaechi BT, Higham SM. Eroded lesions remineralisation by saliva as a possible factor in the site – specificity of human dental erosion. Arch Oral Biol 2001; 46: 697 – 703.
6. Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion. Caries Res 2004; 38: 34 – 44.
7. Attin T, Deifuss H, Hellwig E. Influence of acidified fluoride gel on abrasion resistance of eroded enamel. Caries Res 1999; 33; 135 – 9.
8. Ganss C, Klimek J, Schäffer U, Spall T. Effectiveness of two fluoridation measures on erosion progression in human enamel and dentine in vitro. Caries Res 2001; 35: 325 – 30.
9. Jones L, Lekkas D, Hunt D, McIntyre J, Rafir W. Studies on dental erosion: An in vivo-in vitro model of endogenous dental erosion-its application to testing protection by fluoride gel application. Aust Dent J 2002; 47: 304 – 8.
10. Azzopardi A, Bartlett DW, Watson TF, Sherriff M. The measurement and prevention of erosion and abrasion. J Dent 2001; 29: 393 – 400.
11. Lussi A, Jaeggi T, Schaffner M. Prevention and minimally invasive treatment of erosions. Oral Health Prev Dent 2004; 2: 321 – 5.
12. Yip HK, Lam WTC, Smales RJ. Fluoride release, weight loss and erosive wear of modern aesthetic restoratives. Br Dent J 1999; 187: 265 – 70.
Søkeord for nettversjon: www.tannlegetidende.no: Behandling; Diagnostikk; Forebygging; Tannslitasje
Correspondence: Klinik für Zahnerhaltung, Freiburgstrasse 7, CH – 3010 Bern, Switzerland. E-mail: adrian.lussi@zmk.unibe.ch
Artikkelen er fagfellevurdert.
Artikkelen siteres som:
Lussi A, Schaffner M, Jaeggi T. Dental erosion. Nor Tannlegeforen Tid. 2005;115:160–4. doi:10.56373/2005-3-4